Category Archives: Prescription Drugs
The Chevron Deference Rule: Pay Attention, Health Care Providers! CMS May Lose Control!
It has been nearly 40 years since the Supreme Court indicated in Chevron v. Natural Resources Defense Council that courts should defer to an agency’s reasonable interpretation of an ambiguous statute. Earlier this year, the Supreme Court heard arguments abolishing the Chevron deference rule. It that good or bad? Well, let’s hash it out. Regardless your opinion, the Supreme Court will decide the Chevron deference rule’s legality this summer. And, listening to the oral arguments earlier this year, it seems that a majority of the justices seemed ready to jettison the doctrine or at the very least significantly limit it.
The Chevron deference rule is a critical aspect of administrative law that often remains in the shadows of legal discourse but holds immense implications for the functioning of our government: the Chevron deference rule. This rule, born out of a Supreme Court case in 1984, has been a cornerstone of administrative law, dictating how courts should defer to federal agencies’ interpretations of ambiguous statutes. But as with any legal doctrine, it invites debate, scrutiny, and calls for reform.

In simple terms, the Chevron deference rule mandates that if a statute is ambiguous, courts should defer to the reasonable interpretation of that statute made by the agency tasked with implementing it, unless that interpretation is unreasonable. In essence, it grants federal agencies significant leeway in interpreting laws passed by Congress. This deference has profound effects on the balance of power between the branches of government. For example: CMS is an agency that is allowed deference in its rules that are not laws. See the importance? Without the Chevron deference rule, ALJs would not be bound by CMS’ rules that are not laws. For example, CMS is of the mindsight that extrapolation is legal, allowed, and upheld. The ALJs are bound to agree. No Chevron deference rule? The ALJs can make up their own minds.
The rationale behind Chevron deference is to recognize the expertise of administrative agencies in their respective fields. These agencies possess specialized knowledge and experience that enable them to navigate complex regulatory landscapes. By allowing them deference in interpreting ambiguous statutes, the rule seeks to promote consistency, efficiency, and expertise in policymaking and implementation.
However, as with any legal doctrine, the Chevron deference rule is not without its critics. Some argue that it unduly concentrates power in the hands of unelected bureaucrats, diminishing the role of the judiciary in interpreting the law. Moreover, it raises concerns about accountability and democratic legitimacy, as it can shield agency actions from robust judicial review.
Furthermore, the Chevron deference rule has become a subject of political contention, particularly in recent years. Critics argue that it enables regulatory overreach by agencies, allowing them to enact policies that may exceed the scope of their statutory authority. This concern has led to calls for judicial restraint and a reevaluation of the deference granted to administrative agencies.
So, should the Chevron deference rule stay in place? This question elicits a spectrum of opinions and requires careful consideration. On one hand, the rule promotes efficiency and expertise in governance, recognizing the specialized knowledge of administrative agencies. On the other hand, it raises concerns about accountability, democratic legitimacy, and the balance of power between the branches of government.
In navigating this complex terrain, we must strike a balance that upholds the principles of good governance, accountability, and the rule of law. Perhaps the solution lies not in abolishing the Chevron deference rule altogether but in refining it to address its shortcomings. This could involve clarifying the conditions under which deference is appropriate, ensuring robust judicial oversight, and promoting transparency and accountability in administrative decision-making.
The Chevron deference rule stands as a pivotal element of administrative law, shaping the relationship between the branches of government and influencing the course of public policy. Its effects are profound and far-reaching, touching upon fundamental principles of governance and democracy. As we navigate the complexities of modern governance, let us engage in thoughtful dialogue and debate to ensure that our legal framework reflects the values of accountability, transparency, and the rule of law.
House Bill 403: A Potential Upheaval of Medicaid!
Is this the end of the managed care organizations (MCOs)?
If the Senate’s proposed committee substitute (PCS) to House Bill 403 (HB 403) passes the answer is yes. The Senate’s PCS to House Bill 403 was just favorably reported out of the Senate Health Care Committee on June 15, 2017. The next step for the bill to advance will be approval by the Senate Rules Committee. Click here to watch its progress.
As my readers are well aware, I am not a proponent for the MCOs. I think the MCOs are run by overpaid executives, who pay themselves too high of bonuses, hire charter flights, throw fancy holiday parties, and send themselves and their families on expensive retreats – to the detriment of Medicaid recipients’ services and Medicaid providers’ reimbursement rates. See blog. And blog.
Over the last couple days, my email has been inundated by people abhorred with HB 403 – urging the Senators to retain the original HB 403, instead of the PCS version. As with all legislation, there are good and bad components. I went back and re-read these emails, and I realized multiple authors sat on an MCO Board. Of course MCO Board members will be against HB 403! Instead of hopping up and down “for” or “against” HB 403, I propose a (somewhat) objective review of the proposed legislation in this blog.
While I do not agree with everything found in HB 403, I certainly believe it is a step in the right direction. The MCOs have not been successful. Medically necessary behavioral health care services have been reduced or terminated, quality health care providers have been terminated from catchment areas, and our tax dollars have been misused.
However, I do have concern about how quickly the MCOs would be dissolved and the new PHPs would be put into effect. There is no real transition period, which could provide safety nets to ensure continuity of services. We all remember when NCTracks was implemented in 2013 and MMIS was removed on the same day. There was no overlap – and the results were catastrophic.
The following bullet points are the main issues found in HB 403, as currently written.
- Effective date – MCOs dissolve immediately (This could be dangerous if not done properly)
Past legislation enacted a transition time to dissolve the MCOs. Session Law 2015-245, as amended by Session Law 2016-121, provided that the MCOs would be dissolved in four years, allowing the State to implement a new system slowly instead of yanking the tablecloth from the table with hopes of the plates, glasses, and silverware not tumbling to the ground.
According to HB 403, “on the date when Medicaid capitated contracts with Prepaid Health Plans (PHPs) begin, as required by S.L. 2015-245, all of the following shall occur:…(2) The LME/MCOs shall be dissolved.”
Session Law 2015-245 states the following timeline: “LME/MCOs shall continue to manage the behavioral health services currently covered for their enrollees under all existing waivers, including the 1915(b) and (c) waivers, for four years after the date capitated PHP contracts begin. During this four-year period, the Division of Health Benefits shall continue to negotiate actuarially sound capitation rates directly
with the LME/MCOs in the same manner as currently utilized.”
HB 403 revises Session Law 2015-245’s timeline by the following: “LME/MCOs shall continue to manage the behavioral health services currently covered for their enrollees under all existing waivers, including the 1915(b) and (c) waivers, for four years after the date capitated PHP contracts begin. During this four-year period, the Division of Health Benefits shall continue to negotiate actuarially sound capitation rates directly with the LME/MCOs in the same manner as currently utilized.”
Instead of a 4-year transition period, the day the PHP contracts are effective, the MCOs no longer exist. Poof!! Maybe Edward Bulwer-Lytton was right when he stated, “The pen is mightier than the sword.”
Again, I am not opposed to dissolving the MCOs for behavioral health care; I just want whatever transition to be reasonable and safe for Medicaid recipients and providers.
With the MCOs erased from existence, what system will be put in place? According to HB 403, PHPs shall manage all behavioral health care now managed by MCOs and all the remaining assets (i.e., all those millions sitting in the savings accounts of the MCOs) will be transferred to DHHS in order to fund the contracts with the PHPs and any liabilities of the MCOs. (And what prevents or does not prevent an MCO simply saying, “Well, now we will act as a PHP?”).
What is a PHP? HB 403 defines PHPs as an entity, which may be a commercial plan or provider-led entity with a PHP license from the Department of Insurance and will operate a capitated contract for the delivery of services. “Services covered by PHP:
- Physical health services
- Prescription drugs
- Long-term care services
- Behavioral health services
The capitated contracts shall not cover:
Behavioral healthDentist services- The fabrication of eyeglasses…”
It would appear that dentists will also be managed by PHPs. As currently written, HB 403 also sets no less than three and no more than five contracts between DHHS and the PHPs should be implemented.
Don’t we need a Waiver from the Center for Medicare and Medicaid Services (CMS)?
Yes. We need a Waiver. 42 CFR 410.10(e) states that “[t]he Medicaid agency may not delegate, to other than its own officials, the authority to supervise the plan or to develop or issue policies, rules, and regulations on program matters.” In order to “Waive” this clause, we must get permission from CMS. We had to get permission from CMS when we created the MCO model. The same is true for a new PHP model.
Technically, HB 403 is mandating DHHS to implement a PHP model before we have permission from the federal government. HB 403 does instruct DHHS to submit a demonstration waiver application. Still, there is always concern and hesitancy surrounding implementation of a Medicaid program without the blessing of CMS.
- The provider network (This is awesome)
HB 403 requires that all contracts between PHPs and DHHS have a clause that requires PHPs to not exclude providers from their networks except for failure to meet objective quality standards or refusal to accept network rates.
- PHPs use of money (Also good)
Clearly, the General Assembly drafted HB 403 out of anger toward the MCOs. HB 403 implements more supervision over the new entities. It also disallows use of money on alcohol, first-class airfare, charter flights, holiday parties or similar social gatherings, and retreats, which, we all know these are precisely the activities that State Auditor Beth Wood found occurring, at least, at Cardinal. See Audit Report.
HB 403 also mandates that the Office of State Human Resources revise and update the job descriptions for the area directors and set limitations on salaries. No more “$1.2 million in CEO salaries paid without proper authorization.”
- Provider contracts with the PHPs (No choice is never good)
It appears that HB 403 will not allow providers to choose which PHP to join. DHHS is to create the regions for the PHPs and every county must be assigned to a PHP. Depending on how these PHPs are created, we could be looking at a similar situation that we have now with the MCOs. If the State is going to force you to contract with a PHP to provide Medicaid services, I would want the ability to choose the PHP.
In conclusion, HB 403 will re-shape our entire Medicaid program, if passed. It will abolish the MCO system, apply to almost all Medicaid services (both physical and mental), open the provider network, limit spending on inappropriate items, and assign counties to a PHP.
Boy, what I would give to be a fly on the wall in all the MCO’s boardrooms (during the closed sessions).
Do the Anti-Kickback and Stark Laws Apply to Private Payors?
Good question.
Anti-Kickback statutes (AKS) and Stark law are extremely important issues in health care. Violations of these laws yield harsh penalties. Yet, many healthcare professionals have little to no knowledge on the details of these two legal beasts.
The most common question I get regarding AKS and Stark is: Do AKS and Stark apply to private payers? Health care professionals believe, if I don’t accept Medicare or Medicaid, then I don’t need to worry about AKS and Stark. Are they correct??
The general and overly broad response is that the Stark Law, 42 USC § 1395nn, only applies to Medicare and Medicaid. The AKS, 42 USC § 1320a-7b(b)),applies to any federal healthcare program.
Is there a difference between AKS and Stark?
Answer: Yes. As discussed above, the first difference is that AKS applies to all federal healthcare programs. This stark difference (pun intended) makes the simple decision to not accept Medicare and Medicaid, thus allowing you to never worry about AKS, infinitely more difficult.
Let’s take a step back… What are AKS and Stark laws and what do these laws prohibit? When you Google AKS and Stark, a bunch of legal blogs pop up and attempt to explain, in legalese, what two, extremely esoteric laws purport to say, using words like “renumeration,” “knowing and willful,” and “federal healthcare program.” You need a law license to decipher the deciphering of AKS and Stark. The truth is – it ain’t rocket science.
The AKS is a criminal law; if you violate the AKS, you can be prosecuted as a criminal. The criminal offense is getting something of value for referrals. You cannot refer patients to other health care professionals in exchange for money, reduced rent, use of laboratory equipment, referrals to you, health services for your mother, marketing, weekly meals at Ruth’s Chris, weekly meals at McDonalds, oil changes, discounted theater tickets, Uber rides, Costco coupons, cooking lessons, or…anything of value, regardless the value.
Safe harbors (exceptions to AKS) exist. But those exceptions better fit squarely into the definition of the exceptions. Because there are no exceptions beyond the enumerated exceptions.
AKS is much more broad in scope than Stark. Other than Medicare and Medicaid, AKS applies to any health care plan that utilizes any amount of federal funds. For example, AKS applies to Veterans Health Care, State Children’s Health Programs (CHIP), Federal Employees Health Benefit Program, and many other programs with federal funding. Even if you opt to not accept Medicare and Medicaid, you may still be liable under AKS.
Stark law, on the other hand, is more narrow and only applies to Medicare and Medicaid. I find the following “cheat sheet” created by a subdivision of the Office of Inspector General to be helpful in understanding AKS and Stark and the differences between the two:
One other important aspect of Stark is that is considered “strict liability,” whereas AKS requires a proving of a “knowing and willful” action.
Feel free to print off the above chart for your reference. However, see that little asterisk at the bottom of the chart? It applies here as well.
Turning Medicare Into a Premium Support System: Frequently Asked Questions — The Henry J. Kaiser Family Foundation
Premium support is a general term used to describe an approach to reform Medicare that aims to reduce the growth in Medicare spending. These FAQs raise and discuss basic questions about the possible effects of a premium support system for Medicare beneficiaries, the federal budget, health care providers, and private health plans.
Medicare/Caid Audits: Urine Testing Under Fire!!
I have blogged about peeing in a cup before…but we will not be talking about dentists in this blog. Instead we will be discussing pain management physicians and peeing in a cup.
Pain management physicians are under intense scrutiny on the federal and state level due to increased urine testing. But is it the pain management doctors’ fault?
When I was little, my dad and I would play catch with bouncy balls. He would always play a dirty little trick, and I fell for it every time. He would toss one ball high in the air. While I was concentrating on catching that ball, he would hurl another ball straight at me, which, every time, smacked into me – leaving me disoriented as to what was happening. He would laugh and laugh. I was his Charlie Brown, and he was my Lucy. (Yes, I have done this to my child).
The point is that it is difficult to concentrate on more than one thing. When the Affordable Care Act (ACA) came out, it was as if the federal government wielded 500, metaphoric, bouncy balls at every health care provider. You couldn’t comprehend it in its entirety. There were different deadlines for multiple changes, provider requirements, employer requirements, consumer requirements…it was a bloodbath! [If you haven’t seen the brothers who trick their sister into thinking it’s a zombie apocalypse, you have to watch it!!]
A similar “metaphoric ball frenzy” is occurring now with urine testing, and pain management physicians make up the bulk of prescribed urine testing. The urine testing industry has boomed in the past 4-5 years. This could be caused by a number of factors:
- increase use of drugs (especially heroine and opioids),
- the tightening of regulations requiring physicians to monitor whether patients are abusing drugs,
- increase of pain management doctors purchasing mass-spectrometry machines and becoming their own lab,
- simply more people are complaining of pain, and
- the pharmaceutical industry’s direct-to-consumer advertising (DTCA).
Medicare’s spending on 22 high-tech tests for drugs of abuse hit $445 million in 2012, up 1,423% in five years. “In 2012, 259 million prescriptions were written for opioids, which is more than enough to give every American adult their own bottle of pills.” See article.
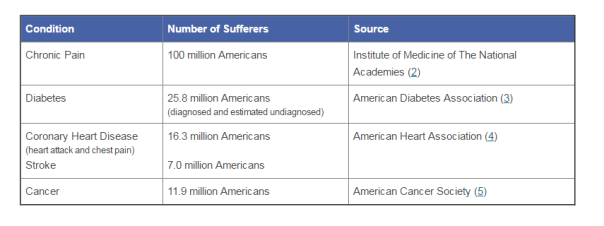
According to the American Association of Pain Management, pain affects more Americans than diabetes, heart disease and cancer combined. The chart below depicts the number of chronic pain sufferers compared to other major health conditions.
In the world of Medicare and Medicaid, where there is profit being made, the government comes a-knockin’.
But should we blame the pain management doctors if recent years brought more patients due to increase of drug use? The flip side is that we do not want doctors ordering urine tests unnecessarily. But aren’t the doctors supposed to the experts on medical necessity??? How can an auditor, who is not a physician and never seen the patient opine to medical necessity of a urine test?
The metaphoric ball frenzy:
There are so many investigations into urine testing going on right now.
Ball #1: The machine manufacturers. A couple of years ago, Carolina Liquid Chemistries (CLC) was raided by the federal government. See article. One of the allegations was that CLC was misrepresenting their product, a urinalysis machine, which caused doctors to overbill Medicare and Medicaid. According to a source, the federal government is still investigating CLC and all the physicians who purchased the urinalysis machine from CLC.
Ball #2: The federal government. Concurrently, the federal government is investigating urine testing billed to Medicare. In 2015, Millennium Health paid $256 million to resolve alleged violations of the False Claims Act for billing Medicare and Medicaid for medically unnecessary urine drug and genetic testing. I wonder if Millennium bought a urinalysis machine from CLC…
Ball #3: The state governments. Many state governments are investigating urine testing billed to Medicaid. Here are a few examples:
New Jersey: July 12, 2016, a couple and their diagnostic imaging companies were ordered to pay more than $7.75 million for knowingly submitting false claims to Medicare for thousands of falsified diagnostic test reports and the underlying tests.
Oklahoma: July 10, 2016, the Oklahoma attorney general’s office announced that it is investigating a group of laboratories involved in the state’s booming urine testing industry.
Tennessee: April 2016, two lab professionals from Bristol, Tenn., were convicted of health care fraud in a scheme involving urine tests for substance abuse treatments.
If you are a pain management physician, here are a few recommendations to, not necessarily avoid an audit (because that may be impossible), but recommendations on how to “win” an audit:
- Document, document, document. Explain why the urine test is medically necessary in your documents. An auditor is less likely to question something you wrote at the time of the testing, instead of well after the fact.
- Double check the CPT codes. These change often.
- Check your urinalysis machine. Who manufactured it? Is it performing accurately?
- Self-audit
- Have an experienced, knowledgeable, health care attorney. Do not wait for the results of the audit to contact an attorney.
And, perhaps, the most important – Do NOT just accept the results of an audit. Especially with allegations involving medical necessity…there are so many legal defenses built into regulations!! You turn around and throw a bouncy ball really high – and then…wallop them!!
RAC Audits: “The Big Bad Wolf” Is Coming to Medicare Advantage…Soon! Beware!
Recovery Audit Contractors (RACs) have been prevalent in traditional Medicare and Medicaid for years now. However, RACs have not knocked on the doors of providers who accept Medicare Advantage yet, despite the Affordable Care Act (ACA) requiring them to do so by 2010. Are RACs going to target Medicare Advantage? Keep reading…
RACs are like the Big Bad Wolf in the “Three Little Pigs.” “Little pig, little pig, let me in!” “Not by the hair of my chinny chin chin!” “Then I’ll huff and puff and blow your house down!”

According to the Center for Medicare and Medicaid Services (CMS), “the Recovery Audit Program’s mission is to identify and correct Medicare improper payments through the efficient detection and collection of overpayments made on claims of health care services provided to Medicare beneficiaries, and the identification of underpayments to providers so that the CMS can implement actions that will prevent future improper payments in all 50 states.”
But the above explanation fails to paint the whole picture.
RACs are compensated by contingency fees. In other words, the more claims they find noncompliant, the more money they are paid. Plus, RACs extrapolate their findings. If a RAC finds $6000 in noncompliant claims, then they extrapolate that number across a universe (usually three years) and come up with some exorbitant number. See blog and blog. The financial incentives create overzealous auditors.
What type of providers accept Medicare Advantage? Advantage providers include optical providers, some durable medical equipment (DME), dentists, nutritionists, and some providers of wellness programs. The Medicare Advantage recipients usually pay a premium. Approximately 15.8 million people rely on Medicare Advantage policies.
CMS has been looking to implement the RAC program on Medicare Advantage for months…if not years. Now, it appears, that the RAC program will be leashed on Medicare Advantage very soon.
“And I’ll blow your house down!!”
CMS released a request for information in December 2015 on how to incorporate RACs into Medicare Advantage, but made little progress until recently.
My “sources” (ha – like I am a journalist) have informed me that the RAC program will soon be released on the Medicare Advantage providers. So be forewarned!!
Don’t be:

Caught with your pants down!
“The Times They Are a-Changin’”: A Look at Possible Ramifications on Medicaid by Senate Bill 744
I think of Bob Dylan’s raspy voice singing:
Then you better start swimmin’
Or you’ll sink like a stone
For the times they are a-changin’.
In 1933, Franklin D. Roosevelt took the presidency during a time of severe poverty. The Great Depression, which would last until the late 1930s or early 1940s, cast shadows and doubt over the future of America. People were starving. Unemployment and homelessness were at an all-time high.
FDR’s first 100 days in office were monumental. In fact, FDR’s first 100 days in office changed America forever. With bold legislation and a myriad of executive orders, he instituted the New Deal. The New Deal created government jobs for the homeless, banking reform, and emergency relief to states and cities. During those 100 days of lawmaking, Congress granted every major request Roosevelt asked. This is an example of what I call blending of the separation of powers. In a time of great national need, Congress took an expansive view of the president’s constitutional powers and cooperated with him to effect major change.
I am in no way comparing our General Assembly to Congress back in the 1930s nor am I comparing FDR to Gov. McCrory. In fact, there are vast differences. I am only making the point that rarely does the legislative body create such change.
But North Carolina’s current Senate Bill 744 may create this change. For example, if Senate Bill 744 passes the House, the Department of Health and Human Services (DHHS), Division of Medical Assistance (DMA) may no longer manage Medicaid. That’s right. A whole new state agency may manage Medicaid.
This past Friday, May 30, 2014, the state Senate passed a $21.2 billion budget, which is known as Senate Bill 744. On May 31, 2014, Senate Bill 744 passed its 3rd reading and will now go on to the House. So far, it has been revised 3 times, so we do not know whether the House will make substantial changes. But, as it stands today, it is shocking. Is it good? Bad? I don’t think we can know whether the changes are good or bad yet, and, quite honestly, I have not had time to digest all of the possible implications of Senate Bill 744. But, regardless, the changes are shocking.
Of the most shocking changes (should SB 744 get passed), consider the following:
1. DHHS must immediately cease all efforts to transition Medicaid to the affordable care organizations (ACOs) system that DHHS had touted would be in effect by July 2015;
2. DHHS’s DMA will no longer manage Medicaid. Instead, a new state entity will be formed to manage Medicaid. (A kind of…”scratch it all and start over” method);
3. All funds previously appropriated to DMA will be transferred to the Office of State Budget and Management (OSBM) and will be used for Medicaid reform and may not be used for any other purpose such as funding any shortfalls in the Medicaid program.
4. Categorical coverage for recipients of the optional state supplemental program State County Special Assistance is eliminated.
5. Coverage for the medically needy is eliminated, except those categories that the State is prohibited from eliminating by the “maintenance of effort” requirement of the Patient Protection and Affordable Care Act. Effective October 1, 2019, coverage for all medically needy categories is eliminated.
6. It is the intent of the General Assembly to reduce optional coverage for certain aged, blind, and disabled persons effective July 1, 2015, while meeting the State’s obligation under the Americans with Disabilities Act and the United States Supreme Court decision in Olmstead v. L.C. ex rel. Zimring, 527 U.S. 581 (1999).
7. Repeal the shared savings program and just reduce the reimbursement rates by 3%.
8. DHHS shall implement a Medicaid assessment program for local management entities/managed care organizations (LME/MCOs) at a rate of three and one-half percent (3.5%).
9. For additional notices as to State Plan Amendments (SPAs), DHHS must post the proposed SPAs on its website at least 10 days prior to submitting the SPAs to the federal Center for Medicare and Medicaid Services (CMS).
10. Reimbursement rate changes become effective when CMS approves the reimbursement rate changes.
11. The Department of Health and Human Services shall not enter into any contract involving the program integrity functions listed in subsection (a) of this section of SB 774 that would have a termination date after September 1, 2015.
12. The Medicaid PROVIDER will have the burden of proof in contested case actions against the Department.
13. The Department shall withhold payment to any Medicaid provider for whom the DMA, or its vendor, has identified an overpayment in a written notice to the provider. Withholding shall begin on the 75th day after the day the notice of overpayment is mailed and shall continue during the pendency of any appeal until the overpayment becomes a final overpayment (can we say injunction?).
Senate Bill 744 purports to make immense modifications to our Medicaid system. I wonder what Gov. McCrory and Secretary Wos think about Senate Bill 744. If SB 744 passes, McCrory and Wos can no longer continue down the ACO path. Does the General Assembly even have the authority to bind their hands from creating ACOs? It seems so.
As for the “new state agency” that will manage Medicaid, maybe the General Assembly is right and we do need to scratch out the current Medicaid management and start over…I doubt anyone would disagree that DHHS has had some “oops” moments in the past year or so. But (a) is this the way to start all over; and (b) does the General Assembly have the legal power to remove the management of Medicaid from Secretary Wos?
Going to the reduction of optional services for the “medically needy,” what services are considered optional? Here is a list of optional services, as defined by the Center of Medicare and Medicaid Services (CMS):
• Case Management
• Mental Health
• Podiatry
• Intermediate Care Facilities (ICF-MR)
• Personal Care Services
• Prosthetics
• Respiratory Therapy
• Hospice
• Adult Dentures
• Prescription Drugs
• Community Alternative Programs (CAP)
• Private Duty Nursing
• Chiropractor
• Home Infusion Therapy
• Physical Therapy/Speech Therapy
• Transportation
I cannot comment on all the changes proposed by Senate Bill 744; I simply have not had enough time to review them in detail, because there are so many changes. I do not purport to know whether these modifications are ultimately for the good or for the bad.
All I know is that we better start swimming or we will sink like a stone, because the times they are a-changin’.




