Monthly Archives: August 2015
Another Win for the Good Guys! Gordon & Rees Succeeds in Overturning Yet Another Medicaid Contract Termination!
Getting placed on prepayment review is normally a death sentence for most health care providers. However, our health care team here at Gordon Rees has been successful at overturning the consequences of prepayment review. Special Counsel, Robert Shaw, and team recently won another case for a health care provider, we will call her Provider A. She had been placed on prepayment review for 17 months, informed that her accuracy ratings were all in the single digits, and had her Medicaid contract terminated.
We got her termination overturned!! Provider A is still in business!
(The first thing we did was request the judge to immediately remove her off prepayment review; thereby releasing some funds to her during litigation. The state is only allowed to maintain a provider on prepayment review for 12 months).
Prepayment review is allowed per N.C. Gen. Stat. 108C-7. See my past blogs on my opinion as to prepayment review. “NC Medicaid: CCME’s Comedy of Errors of Prepayment Review” “NC Medicaid and Constitutional Due Process.”
108C-7 states, “a provider may be required to undergo prepayment claims review by the Department. Grounds for being placed on prepayment claims review shall include, but shall not be limited to, receipt by the Department of credible allegations of fraud, identification of aberrant billing practices as a result of investigations or data analysis performed by the Department or other grounds as defined by the Department in rule.”
Being placed on prepayment review results in the immediate withhold of all Medicaid reimbursements pending the Department of Health and Human Services’ (DHHS) contracted entity’s review of all submitted claims and its determination that the claims meet criteria for all rules and regulations.
In Provider A’s situation, the Carolinas Center for Medical Excellence (CCME) conducted her prepayment review. Throughout the prepayment process, CCME found Provider A almost wholly noncompliant. Her monthly accuracy ratings were 1.5%, 7%, and 3%. In order to get off prepayment review, a provider must demonstrate 70% accuracy ratings for 3 consecutive months. Obviously, according to CCME, Provider A was not even close.
We reviewed the same records that CCME reviewed and came to a much different conclusion. Not only did we believe that Provider A met the 70% accuracy ratings for 3 consecutive months, we opined that the records were well over 70% accurate.
Provider A is an in-home care provider agency for adults. Her aides provide personal care services (PCS). Here are a few examples of what CCME claimed were inaccurate:
1. Provider A serves two double amputees. The independent assessments state that the pateint needs help in putting on and taking off shoes. CCME found that there was no indication on the service note that the in-home aide put on or took off the patients’ shoes, so CCME found the dates of service (DOS) noncompliant. But the consumers were double amputees! They did not require shoes!
2. Provider A has a number of consumers who require 6 days of services per week based on the independent assessments. However, many of the consumers do not wish for an in-home aide to come to their homes on days on which their families are visiting. Many patients inform the aides that “if you come on Tuesday, I will not let you in the house.” Therefore, there no service note would be present for Tuesday. CCME found claims inaccurate because the assessment stated services were needed 6 days a week, but the aide only provided services on 5 days. CCME never inquired as to the reason for the discrepancy.
3. CCME found every claim noncompliant because the files did not contain the service authorizations. Provider A had service authorizations for every client and could view the service authorizations on her computer queue. But, because the service authorization was not physically in the file, CCME found noncompliance.
Oh, and here is the best part about #3…CCME was the entity that was authorizing the PCS (providing the service authorizations) and, then, subsequently, finding the claim noncompliant based on no service authorization.
Judge Craig Croom at the Office of Administrative Hearings (OAH) found in our favor that DHHS via CCME terminated Provider A’s Medicaid contract arbitrarily, capriciously, erroneously, exceeded its authority or jurisdiction, and failed to act as accordingly to the law. He ruled that DHHS’ placement of Provider A on prepayment review was random
Because of Judge Croom’s Order, Provider A remains in business. Plus, she can retroactively bill all the unpaid claims over the course of the last year.
Great job, Robert!!! Congratulations, Provider A!!!
BREAKING: House and Senate appear close to a Medicaid deal!!
In our last post on Medicaid reform, we updated you on the recent bill passed by the North Carolina Senate relating to the long-standing thorn in the side of the General Assembly, especially regarding the states’ budget – the Medicaid program. The Senate’s version of Medicaid reform is quite different from what we have previously seen and is a hodge-podge of managed care and a new idea: “provider-led entities.”
In a strong sign that this proposal is a compromise between competing sides that could end up getting passed, both House and Senate leaders are speaking positively on the record to news media about the prospects for a deal. Given how public the issue is and how big it is (an expected $14.2 billion in North Carolina in the coming year), that means they expect to get a deal done soon. The fact that the issue is so tied up with the budget that is overdue to be passed is a further headwind to passing a bill.
Right now, the bill is in a conference committee of negotiators from the House and Senate to work out an agreement, given the differences between the two chambers.
One major issue that the committee needs to look at is whether there will be a whole new state agency: the “Department of Medicaid.” The Senate endorsed that idea last week.
Our prediction: The legislators will chart a cautious course and not erect a whole new agency at the same time they are overhauling the system.
With Wos having (coincidentally?) just stepped down as Secretary of the Department of Health and Human Services, perhaps the lack of a lightning rod for criticism of DHHS will let the air out of the proposal to remove Medicaid from DHHS’s hands.
Stay tuned.
By Robert Shaw
The Nine Habits of a Highly Effective Secretary for DHHS
With the recent passing of the torch from Aldona Wos to Rick Brajer (see blog), I’ve been thinking about…
What are the qualifications of a Secretary of DHHS?
What exactly are the qualities that would make a great Secretary of DHHS? Remember, in Mary Poppins, when the children draft their requirements for a nanny? Or, better yet, what are the “Seven Habits of a Highly Effective” Secretary for DHHS? Or…in this case, the “Nine Habits”…
Here are my “Nine Habits of a Highly Effective Secretary of DHHS;” our Secretary of DHHS should have the following:
- A health care background
- A successful track record of his/her ability to manage large companies or agencies
- An understanding of the Medicaid system, and, maybe, even have first-hand knowledge of how the system affects recipients and providers
- A relationship with someone on Medicaid or a parent of someone on Medicaid
- A working knowledge of clinical coverage policies, reimbursement rates, and regulations surrounding Medicaid
- Both the capacity to listen and speak and do both eloquently and genuinely
- True empathy about the physical and mental health of Medicaid recipients and about providers, plus have the patience to handle all types of demographic differences
- An understanding that he/she is handling tax payers’ money, that redundancy in staff is excess administrative costs, and ability to trim the fat
- An ability to communicate with both the Senate and the House and to be frank with both
Let us analyze the qualifications of Wos that we came to witness over the last few years, as well as, review the qualifications of soon-to-be Sec. Brajer with information to which we are privy.
Let’s see if both, either, or neither have these “Nine Habits of a Highly-Effective Secretary for DHHS.”
- Health care background:
Wos: Yes. And, yet, maybe not. She is an M.D. Although I do not know whether she ever practiced medicine in North Carolina. According to Wikipedia, (which is never wrong) Wos “prides herself on her work in the field of preventing HIV and AIDS.” However, I was unable to find a single clinic in which Wos provided services. While, generally, an “M.D.” automatically bestows a certain aura of understanding health care, I question whether this “M.D.” automatically has a working knowledge of billing for and receiving reimbursements under Medicaid in North Carolina.
Brajer: Hmmmm. This one is more tricky. The two companies that Brajer owned, Pro-nerve LLC and LipoScience Inc., are health care related, in that Pro-nerve was an intraoperative neuromonitoring (IONM) company and LipoScience sold a diagnostic tool to health care providers. Arguably, both companies are health care related, at least, in an ancillary way. However, Brajer is not a health care professional, and, to my knowledge, has never rendered health care services. Furthermore, neither of Brajer’s companies was successful; quite the opposite is true, in fact. From my understanding, one company declared bankruptcy and the other was not far behind. Which brings us to the next category…
Answer: Both…kinda.
2. A successful track record of his/her ability to manage large entities:
Wos: Prior to acting as the Secretary to DHHS, Wos served as the Ambassador to Estonia until 2006. What she did besides political functions between 2006 and 2012, I do not know. Acting as an Ambassador does not entail managing large entities. The most managerial skills that I can find in her background, prior to being appointed Secretary, are related to political fund-raising. Since I would not call her brief reign as Secretary of DHHS a success, I give Wos a “two thumbs down” on this criterion.
Brajer: He managed two companies. We can bicker as to whether these companies should be considered large…neither employed 17,000 employees. Regardless, the “successful” criterion appears to be lacking.
Answer: Neither…pickles.
3. An understanding of the Medicaid system:
Wos: “You’re asking me without having all the data available to answer a question,” she told lawmakers on October 8, 2013. In her defense, she responded as such when asked whether the State was moving toward privatization for Medicaid. No one could know the answer, except, maybe, McCrory.
On the other hand, the implementation of NCTracks was nothing short of a catastrophe of epic proportion. See blog. See blog. Anyone with nominal knowledge of the Medicaid system would have, at least, paused to consider keeping HP Enterprises under contract during the switch to NCTracks or pushed back the go-live date.
Brajer: Unknown
Answer: Here’s to hoping that Brajer does. I’m cheering for you! Go! Fight! Win!
4. A relationship with someone on Medicaid or a parent of someone on Medicaid:
Wos: Unknown. If I were shaking a proverbial “8 Ball,” it would read, “Doubtful.”
Brajer: Unknown. Perhaps one of his former employees at Pro-nerve, LLC and LipoScience, Inc. is on Medicaid.
Answer: Gimme a ‘B’! B! Gimme a ‘R’! R! Gimme a ‘A’! A! Gimme a ‘J’! J! Gimme a ‘E’! E! Gimme a ‘R’! R! Whats that spell? Brajer!!
5. A working knowledge of clinical coverage policies, reimbursement rates, and regulations surrounding Medicaid.
Wos: Unknown. Whatever Wos’ knowledge of regulations and clinical coverage policies is or lacked, she, initially, made up for any knowledge lacked with the key hire and quick resignation of Carol Steckel. Unfortunately, Steckel’s experience was never replaced.
January 2013: “I am pleased to say that we are already taking steps to address some of these issues,” Wos said. “Now, the most important of this is that we have hired Ms. Carol Steckel, a nationally recognized — nationally recognized — expert in Medicaid to run our Medicaid program for the state. Carol is already moving ahead with systemic reviews of operations in this division. She is reviewing and establishing new policies and procedures.”
September 27, 2013: Steckel resigns. And blog.
Brajer: Unknown.
Answer: B! R! A! J! E! R! Let’s go, Brajer!
6. Both the capacities to listen and speak and do both eloquently.
Wos: Wos brandished an ability to speak publicly with ease. Listening, on the other hand….eh?
Brajer: Unknown
Answer: I think you can, I think you can, I think you can…
7. Genuine concern about the physical and mental health of Medicaid recipients AND about providers PLUS have the patience to handle all types of demographic differences
Wos: She seems to think so. Her country club does not discriminate.
Brajer: Unknown
Answer: Go! Go! Go! Go! Go, Brajer!!
8. An understanding that he/she is handling tax payers money and that redundancy in staff is excess administrative costs and trim the meat
Wos: “My obligation as secretary is to find the best possible team in order to get the job done.” Les Merritt served as CFO of DMA on a $300,000-plus contract. Joe Hauck was paid over $228,000 for 6 months of advise to Wos. Matt McKillip was paid $87,500 to serve as chief policy maker without any health care background. Ricky Diaz pulled in $85,000 as communications director. Id. Wos has handed out $1.7 million in pay hikes to 280 staffers, many with “no career or educational experience for the jobs they hold.” Id. The implementation of the MCOs also fell under Wos’ watchful eye. The MCO system has created thousands upon thousands of high-paying jobs with our Medicaid dollars. I believe that in the “trim the fat” category, Sec. Wos scores a goose egg.
Brajer: Unknown.
Answer: Please, Brajer! For the love of Pete!
9. Ability to communicate with both the Senate and the House and to be frank with both.
Wos: “Separation pay” v. “Severance pay?”
In April 2013: “I think the word transparency can get pretty dangerous,” Wos said. “Because what does transparency mean? If transparency means that we’re in a planning process and you’re asking us, ‘Tell us all the things you’re planning,’ well, my goodness, allow us to work, and then we’ll give you everything that you want.”
Brajer: Unknown
Answer: Brajer, Brajer, He’s our man! If he can’t do it…[gulp].
____________________________________________
It concerns me that so many of future Sec. Brajer’s core abilities/habits to run and manage DHHS and the Medicaid program in a highly effective manner are unknown. Nothing like placing all your money on red! But we have HIGH hopes for Brajer!!! Don’t let us down!!
The whole point of this blog is to pause and really contemplate what characteristics would comprise a great Secretary for DHHS. Obviously, the Governor has the full authority to appoint the Secretary, meaning that we taxpayers have little to no input as to whether we deem a person qualified, except in the indirect method of voting or not voting for the Governor.
Call this blog an exercise in examining what habits, if in existence, would make the most highly effective Secretary of DHHS and an opinion as to whether these habits exist in our former and future Secretaries.
We are cheering for Brajer! But…
One fact about the future is that it is unknown.
North Carolina Medicaid Reform Update – Round and Round She Goes
Given how long the Medicaid reform discussions have been going on at the legislature, you may be glazed over by now. Give me the memo when they pass something, right? Fair enough, let’s keep it brief. Where do things stand right now?
Last Wednesday, the Senate staked out its position in the ongoing debate between the House and the McCrory administration.
The Senate’s newest proposal is an unusual mix of different systems and new ideas. Not willing to commit to one model for the whole Medicaid program, the latest version of the bill includes something new called Provider Led Entities, or “PLEs.” PLEs are yet the latest in the alphabet soup of different alternatives to straight fee-for-service billing for Medicare/Medicaid. You’ve all heard of HMOs, PPOs, MCOs, and ACOs. PLEs appear to be similar to ACOs, but perhaps for political reasons the Senate bill sponsors saw the need to call the idea something different. See Knicole Emanuel’s blog.
In any event, as the name suggests, such organizations would be provider-led and would be operated through a capitated system for managing the costs of the Medicaid program. The Senate bill would result in up to twelve PLEs being awarded contracts on a regional basis.
PLEs are not the only addition to the Medicaid alphabet soup that the Senate is proposing in its version of HB 372. The Senate has also renewed its interest in taking Medicaid out of the hands of the N.C. Department of Health and Human Services entirely and creating a new state agency, the Department of Medicaid (“DOM”).
(One wonders whether the continual interest in creating a new Department of Medicaid independent of the N.C. Department of Health and Human Services had anything to do with embattled DHHS Secretary Wos stepping down recently.)
The Senate also proposes creating a Joint Legislative Oversight Committee on Medicaid (“LOC on Medicaid”).
But creating the DOM and using new PLEs to handle the provision of Medicaid services is not the whole story. Perhaps unwilling to jump entirely into a new delivery system managed by a wholly new state agency, the Senate bill would keep LME/MCOs for mental health services in place for at least another five years. Private contractor MCOs would also operate alongside the PLEs. The North Carolina Medicaid Choice coalition, a group which represents commercial MCOs in connection with the Medicaid reform process, is pleased.
One very interesting item that the Senate has included in its proposed legislation is the following requirement: “Small providers shall have an equal opportunity to participate in the provider networks established by commercial insurers and PLEs, and commercial insurers and PLEs shall apply economic and quality standards equally regardless of provider size or ownership.” You can thank Senator Joel Ford of Mecklenburg County for having sponsored this amendment to the Senate version of House Bill 372.
By pulling the Medicaid reform proposal out of the budget bill, the matter appears headed for further negotiation between the House and the Senate to see if the two can agree this year, unlike last year.
By legislative standards, that counts as forward progress… Here come the legislative discussion committees to hash it out more between the two chambers. We will keep a close eye on the proposals as they continue to evolve.
By Robert Shaw

False Claims Act: The Medicare Horror Story
What the heck is the False Claims Act and why is it important to you?
When it comes to Medicaid and Medicare, the ghoulish phrase “False Claims Act” is frequently thrown around. If you google False Claims Act (FCA) under the “news” option, you will see some chilling news article titles.
- Pediatric Services of America, units to pay $6.88 in False Claims
- NuVasive, Inc. Agrees to Pay $13.5 Million to Resolve False Claims
- California Oncologist Pays $736k to Settle False Claims Allegations
False claims cases tend to be high dollar cases for health care providers; many times the amounts are at issue that could potentially put the provider out of business. FCA is spine-chilling, and many health care providers would rather play the hiding child rather than the curious investigator in a horror story. Come on, let’s face it, the curious characters usually get killed. But, this is not a horror story, and it is imperative that providers are informed of the FCA and potential penalties.
I have blogged about post payment reviews that use extrapolation, which result in astronomical alleged overpayments. See blog and blog. Interestingly, these alleged overpayments could also be false claims. It is just a matter of which governmental agency is pursuing it (or person in the case of qui tem cases).
But the ramifications of false claims allegations are even more bloodcurdling than the astronomical alleged overpayments. It is important for you to understand what false claims are and how to prevent yourself from ever participating in a false claim, knowingly or unknowingly.
First, what is a false claim?
A false claims occurs when you knowingly present, or cause to be presented, to the US Government a false or fraudulent claim for payment or approval. (abridged version).
Let’s analyze.
The false claim does not have to be billed with actual knowledge that it is false or fraudulent. The false claim does not even have to be fraudulent; it can be merely false. The distinction lies in that a fraudulent claim is one that you intentionally alter. A false claim could merely be incorrect information. Saying it another way, the false claim can be a false or incorrect claim that you had no actual knowledge was false. That is hair-raising.
What is the penalty? It is:
A civil penalty of not less than $5,500 and not more than $11,000 per claim, plus 3 times the amount of the claim. You can see why these are high dollar cases.
The federal government recovered a jaw-dropping $5.7 billion in 2014 under the False Claims Act (FCA). In 2013, the feds recovered $5 billion under the FCA. Expect 2015 to be even higher. Since the inception of the Affordable Care Act (ACA), FCA investigations have increased.
Overwhelmingly, the recoveries are from the health care industry.
Everyone knows that the Medicare Claims Processing Manual is esoteric, verbose, and vague. Let’s face it: just Chapter 1 “General Billing Requirements” alone is 313 pages! Besides me, who reads the Medicare Claims Processing Manual cover to cover? Who, besides me, needs to know that Medicare does not cover deported beneficiaries or the exceptions to the Anti-markup Payment Limitation?
Not to mention, the Manual is not law. The Manual does not get approved by Congress. The Manual is guidance or policy.
However, in FCA cases, you can be held liable for items in the Medicare Claims Processing Manual of which you were not aware. In other words, in FCA cases, you can be found liable for what you should have known.
Real life hypotheticals:
Hospital submits claims to Medicare and received payment for services rendered in a clinical trial involving devices to improve organ transplants. Unbeknownst to the hospital, the Manual prohibits Medicare reimbursements for non-FDA approved services.
Physician A has reciprocal arrangement with Physician B. A undergoes personal surgery and B serves A’s Medicare Part B patients while A is recovering. A returns and bills Medicare and is paid for services rendered by B 61 days+ after A left the office.
A physician accepts assignment of a bill of $300 for covered Medicare services and collects $80 from the enrollee. Physician neglects to depict on the claim form that he/she collected anything from the patient. Medicare’s allowable amount is $250, and since the deductible had previously been met, makes payment of $200 to the physician.
These are just a few examples of situations which could result in a FCA allegation.
But do not fret! There are legal defenses written into the Social Security Act that provides protection for health care providers!
Important take-aways:
1. Check whether you have insurance coverage for FCA.
2. Have an attorney on hand with FCA experience.
3. Read portions of the Medicare Claims Billing Manual which are pertinent to you.
Most importantly, if you are accused of billing false claims, get your advocate sooner rather than later! Do not engage in any conversations or interviews without counsel!
Appeal all findings!
Passing the Torch: Wos Resigns!! Brajer Appointed!
Aldona Wos resigned today after two years and seven months as Secretary of NC DHHS. Wos’ last day will be Aug. 14.
McCrory named Rick Brajer, a former medical technology executive, as the new Secretary of DHHS.
Soon-to-be Sec. Brajer, 54, was the chief executive of ProNerve and LipoScience. LipoScience was sold to LabCorp in 2014, and ProNerve was sold to Specialty Care in April.
Brajer is not a doctor, as Wos was. Instead, Brajer touts an MBA from Stanford.
I do not have any information as to why Wos resigned now, especially in light of the recent resignation of the Secretary of Transportation, but will keep you apprised.
More to come….
Consider Nominating This Blog for the 2015 Best Legal Blog Contest (Please)!
The 2015 Legal Blog Contest is here!
For all you that follow this blog, thank you! I hope that you agree that I provide you with valuable and up-to-date information on Medicaid/care regulatory issues. At least, that is my hope in maintaining this blog. And maintaining this blog takes a lot of time outside my normal, hectic legal career and my time as a mom and wife. Don’t get me wrong…I love blogging about these issues because these issues are near and dear to my heart. I am passionate about health care, health care providers, Medicaid and Medicare, and access to quality care.
If you are a follower, then you know that I try to keep my readers current on Medicaid/care fraud, federal and state laws, legal rights for health care providers, bills in the General Assembly germane to health care, extrapolation issues, CMS rulings, managed care matters, reimbursement rates, RAC audits and much, much more!
If you enjoy my blog, I ask a favor. Please consider nominating my blog for the 2015 Best Legal Blog Contest.
If you want to nominate my blog, please click here.
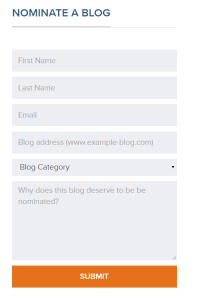
Scroll down until you see this:
Enter your name, email address, my blog address. which is:
For category, click on “Niche and Specialty.” I do not believe the other categories correctly describe my blog.
And type a reason why you enjoy my blog. Much appreciated!