Blog Archives
NC Medicaid OVERHAULED!
NC Medicaid is getting a complete overhaul. Politically, everyone is lost and has no idea how this will work. Back in 2010-ish, when NC went to the MCO model, which we have now, hundreds of providers were not paid or had trouble getting paid until the “dust” settled, and the MCOs were familiar with their jobs. Providers continue to suffer nonpayment from MCOs.
The new model consists of two, separate models: (1) the Standard Plan; and (2) the Tailored Plan models.
What’s the difference?
The Tailored Plan
Applies to:
- People who get Innovations Waiver services
- People who get Traumatic Brain Injury (TBI) Waiver services
- People who may have a mental health disorder,substance use disorder, intellectual /developmental disability (I/DD) or traumatic brain injury (TBI).
The Standard Plan
Applies to everyone else. It is normal, physical Medicaid.
December 1, 2022, is the “go-live” date for the Tailored Plans.
Unlike the MCO model, the Tailored Plan offers physical health, pharmacy, care management and behavioral health services. It is for members who may have significant mental health needs, severe substance use disorders, intellectual/developmental disabilities (I/DDs) or traumatic brain injuries (TBIs). Tailored Plans offer added services for members who qualify. DHHS is trying to distance itself from any Medicaid administration by hiring all these private companies to manage Medicaid for DHHS. DHHS has to get federal Waivers to do this.
The MCOs are taking on a new function. Starting December 1, 2022, the MCOs will be managing physical care, as well as mental health and substance abuse.
I see this HUGE change as good and bad (isn’t everything?). The good side effect of this transition is that Medicaid recipients who suffer mental health and/or substance abuse will have their physical health taken care of by the same MCO that manage their mental health and/or substance abuse services. Despite, this positive side effect, we all know that whenever NC Medicaid is OVERHAULED, consumers fall between cracks on a large scale. Let’s just hope that this transition will be easier than past transitions.
Dave Richard, Deputy Secretary NC Medicaid, NCDHHS, gave a presentation today for the NCSHCA. He said that the transition to MCOs was rocky. What does he think will happen when we transfer to the Tailored Plan?
I think I may ask him whether he thinks whether the MCOs are doing a good job, presently.
He’s a great presenter.
He said that the hospitals have come together in the last 4 weeks. He said that we will see something in the media on Monday.
He wants to expand Medicaid because his agency DHHS would be awarded $1.5 Billion over the course of 2 years. Of course, he wants to expand. He has no idea that the MCOs are “terminating at will” providers within the catchment areas in a disproportionate and discriminatory way.
We are close to expansion, he said. 80%, he guessed. “Expansion is really important.”
Not if there are not enough providers.
I did not ask him my question.
Today Mr. Richard had to get a bunch of data from the “new plans.” We are 2 1/2 months away, and he said they are not prepared yet, but hopes to be prepared by December 1, 2022. They still have the discretion to “pull the plug.” He’s worried about a lot of providers who have invested a lot of money to get compliant and ready for the transformation – that they won’t get paid.
“We have 5 really, strong Standard Plans,” he said. Most Medicaid recipients will choose the 5 Standard Plans,
Attorney from the audience: “We have to raise reimbursement rates.” There is a staffing crisis, the attorney, emphasized.
Mr. Richard stated that there will be a raise, but no indication of how much.
Finally, I did ask him his opinion as to whether he thinks the MCOs are doing better now than when the transformation happened (back in 2010-ish).
He said, that nothing is perfect. And that other Medicaid Deputy Secretaries think very highly of NC’s program. I wonder if he’ll run for office. He would win.
The guy next to me asked, “What is the future of the Tailored Plans when they go out of business in 4 years?”
Mr. Richards said that there needed to be competition for being the “big dogs.”
Medicaid Reform: As Addictive as Fortnite
Do you have a kid addicted to Fortnite? The numbers are rising…
For those of you who have been living under a rock for the past year, this is how Fortnite is explained on the internet:
“In short, it’s a mass online brawl where 100 players leap out of a plane on to a small island and then fight each other until only one is left. Hidden around the island are weapons and items, including rifles, traps and grenade launchers, and players must arm themselves while exploring the landscape and buildings. It’s also possible to collect resources that allow you to build structures where you can hide or defend yourself. As the match progresses, the playable area of land is continually reduced, so participants are forced closer and closer together. The last survivor is the winner.”
More than 40 million people play Fortnite. According to the May 2018 Medicaid Enrollment Report, 73,633,050 Americans are enrolled in Medicaid or CHIP, so government-assisted health insurance definitely trumps Fortnite on participation.
Recently, the General Assembly passed and the Governor signed two Bills into law pertaining to Medicaid reform: (1) HB 403 (Session Law 2018-48); and (2) HB 156 (Session Law 2018-49). Notice that the Session Laws are one digit separate from each other. That is because Governor Cooper signed these two bills consecutively and on the same day. But did he read them? I do not know the answer, but I do know this: Medicaid reform in NC has become a Fortnite. The MCOs, provider-led entities, ACOs, auditors, DHHS…everyone is vying for a piece of the very large Medicaid budget, approximately $3.6 billion – or 16% of NC’s total budget. It is literally a firehose of money if you can manage to be a player in the Medicaid Fortnite – a fight to eliminate everyone but you. Unlike Fortnite, the pay-off for winning Medicaid Fortnite is financially lucrative. But it is a fight with few winners.
Session Law 2018-48 is entitled, “An Act to Modify the Medicaid Transformation Legislation.”
Session Law 2018-49 is entitled, “An Act to Require Medicaid Prepaid Health Plans to Obtain a License from the Department of Insurance and to Make Other Changes Pertaining to Medicaid Transformation and the Department of Insurance.”
Don’t you like how the House decided to use the term “transformation” instead of “reform?” The term “reform” had been over-utilized.
Recently, the North Carolina Medical Society announced that it is throwing its metaphoric hat in the ring to become “Carolina Complete Health,” a provider-led patient-care center.
The New Laws
Session Law 2018-48
Session Law 2018-48 defines provider-led entity (PLE) as an entity that meets the following criteria: (1) A majority of the entity’s ownership is held by an individual or entity that has its primary business purpose the operation of a capitated contract for Medicaid; (2) A majority of the entity’s governing body is composed of licensed physicians, physician assistants, nurse practitioners, or psychologist and have experience treating Medicaid beneficiaries; (3) Holds a PHP license issued by the Department of Insurance (see Session Law 2018-49).
Services covered by PHP’s will include physical health services, prescription drugs, long-term services and supports, and behavioral health care services for North Carolina Health Choice recipients. The PHP’s will not cover services currently covered by the managed care organizations (MCOs).
Session Law 2018-48 allows for 4 contracts with PHPs to provide services for Medicaid and NC Health Choice (statewide contracts). Plus, it allows up to 12 regional contracts.
What is the future of behavioral health and the MCO system?
For now, they will still exist. The double negative wording of the new Session Law makes it seem like the MCOs will have less authority, but the MCOs will continue to cover for services described in subdivisions a, d, e, f, g, j, k, and l of this subdivision.
Session Law 2018-48 also creates new entities called BH IDD Tailored Plans. Session Law 2018-48 carves out developmentally disabled services (or IDD). It mandates that DHHS create a detailed plan for implementation of a new IDD program under the 1115 Waiver. Services provided by the new Tailored Plans shall pay for and manage services currently offered under the 1915(b)(c) Waiver.
Here’s the catch for providers: “Entities operating BH IDD Tailored Plans shall maintain closed provider networks for behavioral health, intellectual and developmental disability, and traumatic brain injury services and shall ensure network adequacy.” (emphasis added). Fortnite continues with providers jockeying to be included in the networks.
For the next four years only an MCO may operate a BH IDD Tailored Plan. This tells me that the MCOs have sufficiently lawyered up with lobbyists. After the term of the initial contracts, the Tailored Plans will be the result of RFPs issued by DHHS and the submission of competitive bids from nonprofit PHPs.
DHHS was to report to the Joint Legislative Oversight Committee with a plan for the implementation of the Tailored Plans by June 22, 2018. – Sure would’ve loved to be a fly on that wall.
Starting August 31, 2018, DHHS is authorized to take any actions necessary to implement the BH IDD Tailored Plans in accordance with all the requirements in this Act.
Session Law 2018-49
A provider-led entity must meet all the following criteria: (1) A majority of the entity’s ownership is held by an individual or entity that has as its primary business purpose operating a capitated contract with with Medicaid providers; and (2) A majority of the governing body is composed of individuals who are licensed as physicians, physician assistants, nurse practitioners, or psychologists and all of whom have experienced treating Medicaid beneficiaries.
Session Law 2018-49 requires that all PHPs apply for a license with the Commissioner of Insurance. With the application, all entities would need to provide proof of financial stability and other corporate documents. This new law definitely increases the authority of the Commissioner of Insurance (Mike Causey).
The remaining portion of the law pertains to protection against insolvency, continuation of healthcare services in case of insolvency, suspension or revocation of licenses, administrative procedures, penalties and enforcement, confidentiality of information, and that sort.
Session Law 2018-49 also applies to the current opioid crisis. It allows a “lock-in programs” for those consumers who use multiple pharmacies and multiple doctors to “lock them in” to one pharmacy and one doctor.
Besides the “lock-in” program, Session Law 2018-49 is basically a law that brings the Department of Insurance into the Medicaid arena.
Let Fortnite begin!
House Bill 403: A Potential Upheaval of Medicaid!
Is this the end of the managed care organizations (MCOs)?
If the Senate’s proposed committee substitute (PCS) to House Bill 403 (HB 403) passes the answer is yes. The Senate’s PCS to House Bill 403 was just favorably reported out of the Senate Health Care Committee on June 15, 2017. The next step for the bill to advance will be approval by the Senate Rules Committee. Click here to watch its progress.
As my readers are well aware, I am not a proponent for the MCOs. I think the MCOs are run by overpaid executives, who pay themselves too high of bonuses, hire charter flights, throw fancy holiday parties, and send themselves and their families on expensive retreats – to the detriment of Medicaid recipients’ services and Medicaid providers’ reimbursement rates. See blog. And blog.
Over the last couple days, my email has been inundated by people abhorred with HB 403 – urging the Senators to retain the original HB 403, instead of the PCS version. As with all legislation, there are good and bad components. I went back and re-read these emails, and I realized multiple authors sat on an MCO Board. Of course MCO Board members will be against HB 403! Instead of hopping up and down “for” or “against” HB 403, I propose a (somewhat) objective review of the proposed legislation in this blog.
While I do not agree with everything found in HB 403, I certainly believe it is a step in the right direction. The MCOs have not been successful. Medically necessary behavioral health care services have been reduced or terminated, quality health care providers have been terminated from catchment areas, and our tax dollars have been misused.
However, I do have concern about how quickly the MCOs would be dissolved and the new PHPs would be put into effect. There is no real transition period, which could provide safety nets to ensure continuity of services. We all remember when NCTracks was implemented in 2013 and MMIS was removed on the same day. There was no overlap – and the results were catastrophic.
The following bullet points are the main issues found in HB 403, as currently written.
- Effective date – MCOs dissolve immediately (This could be dangerous if not done properly)
Past legislation enacted a transition time to dissolve the MCOs. Session Law 2015-245, as amended by Session Law 2016-121, provided that the MCOs would be dissolved in four years, allowing the State to implement a new system slowly instead of yanking the tablecloth from the table with hopes of the plates, glasses, and silverware not tumbling to the ground.
According to HB 403, “on the date when Medicaid capitated contracts with Prepaid Health Plans (PHPs) begin, as required by S.L. 2015-245, all of the following shall occur:…(2) The LME/MCOs shall be dissolved.”
Session Law 2015-245 states the following timeline: “LME/MCOs shall continue to manage the behavioral health services currently covered for their enrollees under all existing waivers, including the 1915(b) and (c) waivers, for four years after the date capitated PHP contracts begin. During this four-year period, the Division of Health Benefits shall continue to negotiate actuarially sound capitation rates directly
with the LME/MCOs in the same manner as currently utilized.”
HB 403 revises Session Law 2015-245’s timeline by the following: “LME/MCOs shall continue to manage the behavioral health services currently covered for their enrollees under all existing waivers, including the 1915(b) and (c) waivers, for four years after the date capitated PHP contracts begin. During this four-year period, the Division of Health Benefits shall continue to negotiate actuarially sound capitation rates directly with the LME/MCOs in the same manner as currently utilized.”
Instead of a 4-year transition period, the day the PHP contracts are effective, the MCOs no longer exist. Poof!! Maybe Edward Bulwer-Lytton was right when he stated, “The pen is mightier than the sword.”
Again, I am not opposed to dissolving the MCOs for behavioral health care; I just want whatever transition to be reasonable and safe for Medicaid recipients and providers.
With the MCOs erased from existence, what system will be put in place? According to HB 403, PHPs shall manage all behavioral health care now managed by MCOs and all the remaining assets (i.e., all those millions sitting in the savings accounts of the MCOs) will be transferred to DHHS in order to fund the contracts with the PHPs and any liabilities of the MCOs. (And what prevents or does not prevent an MCO simply saying, “Well, now we will act as a PHP?”).
What is a PHP? HB 403 defines PHPs as an entity, which may be a commercial plan or provider-led entity with a PHP license from the Department of Insurance and will operate a capitated contract for the delivery of services. “Services covered by PHP:
- Physical health services
- Prescription drugs
- Long-term care services
- Behavioral health services
The capitated contracts shall not cover:
Behavioral healthDentist services- The fabrication of eyeglasses…”
It would appear that dentists will also be managed by PHPs. As currently written, HB 403 also sets no less than three and no more than five contracts between DHHS and the PHPs should be implemented.
Don’t we need a Waiver from the Center for Medicare and Medicaid Services (CMS)?
Yes. We need a Waiver. 42 CFR 410.10(e) states that “[t]he Medicaid agency may not delegate, to other than its own officials, the authority to supervise the plan or to develop or issue policies, rules, and regulations on program matters.” In order to “Waive” this clause, we must get permission from CMS. We had to get permission from CMS when we created the MCO model. The same is true for a new PHP model.
Technically, HB 403 is mandating DHHS to implement a PHP model before we have permission from the federal government. HB 403 does instruct DHHS to submit a demonstration waiver application. Still, there is always concern and hesitancy surrounding implementation of a Medicaid program without the blessing of CMS.
- The provider network (This is awesome)
HB 403 requires that all contracts between PHPs and DHHS have a clause that requires PHPs to not exclude providers from their networks except for failure to meet objective quality standards or refusal to accept network rates.
- PHPs use of money (Also good)
Clearly, the General Assembly drafted HB 403 out of anger toward the MCOs. HB 403 implements more supervision over the new entities. It also disallows use of money on alcohol, first-class airfare, charter flights, holiday parties or similar social gatherings, and retreats, which, we all know these are precisely the activities that State Auditor Beth Wood found occurring, at least, at Cardinal. See Audit Report.
HB 403 also mandates that the Office of State Human Resources revise and update the job descriptions for the area directors and set limitations on salaries. No more “$1.2 million in CEO salaries paid without proper authorization.”
- Provider contracts with the PHPs (No choice is never good)
It appears that HB 403 will not allow providers to choose which PHP to join. DHHS is to create the regions for the PHPs and every county must be assigned to a PHP. Depending on how these PHPs are created, we could be looking at a similar situation that we have now with the MCOs. If the State is going to force you to contract with a PHP to provide Medicaid services, I would want the ability to choose the PHP.
In conclusion, HB 403 will re-shape our entire Medicaid program, if passed. It will abolish the MCO system, apply to almost all Medicaid services (both physical and mental), open the provider network, limit spending on inappropriate items, and assign counties to a PHP.
Boy, what I would give to be a fly on the wall in all the MCO’s boardrooms (during the closed sessions).
Work Requirements for Medicaid?
Under the Trump Administration, some Republican governors may look to move their Medicaid programs in a more conservative direction. In his latest column for Axios, Drew Altman discusses the arguments about Medicaid “work requirements” and why few people are likely to be affected by them in practice.
BREAKING: House and Senate appear close to a Medicaid deal!!
In our last post on Medicaid reform, we updated you on the recent bill passed by the North Carolina Senate relating to the long-standing thorn in the side of the General Assembly, especially regarding the states’ budget – the Medicaid program. The Senate’s version of Medicaid reform is quite different from what we have previously seen and is a hodge-podge of managed care and a new idea: “provider-led entities.”
In a strong sign that this proposal is a compromise between competing sides that could end up getting passed, both House and Senate leaders are speaking positively on the record to news media about the prospects for a deal. Given how public the issue is and how big it is (an expected $14.2 billion in North Carolina in the coming year), that means they expect to get a deal done soon. The fact that the issue is so tied up with the budget that is overdue to be passed is a further headwind to passing a bill.
Right now, the bill is in a conference committee of negotiators from the House and Senate to work out an agreement, given the differences between the two chambers.
One major issue that the committee needs to look at is whether there will be a whole new state agency: the “Department of Medicaid.” The Senate endorsed that idea last week.
Our prediction: The legislators will chart a cautious course and not erect a whole new agency at the same time they are overhauling the system.
With Wos having (coincidentally?) just stepped down as Secretary of the Department of Health and Human Services, perhaps the lack of a lightning rod for criticism of DHHS will let the air out of the proposal to remove Medicaid from DHHS’s hands.
Stay tuned.
By Robert Shaw
North Carolina Medicaid Reform Update – Round and Round She Goes
Given how long the Medicaid reform discussions have been going on at the legislature, you may be glazed over by now. Give me the memo when they pass something, right? Fair enough, let’s keep it brief. Where do things stand right now?
Last Wednesday, the Senate staked out its position in the ongoing debate between the House and the McCrory administration.
The Senate’s newest proposal is an unusual mix of different systems and new ideas. Not willing to commit to one model for the whole Medicaid program, the latest version of the bill includes something new called Provider Led Entities, or “PLEs.” PLEs are yet the latest in the alphabet soup of different alternatives to straight fee-for-service billing for Medicare/Medicaid. You’ve all heard of HMOs, PPOs, MCOs, and ACOs. PLEs appear to be similar to ACOs, but perhaps for political reasons the Senate bill sponsors saw the need to call the idea something different. See Knicole Emanuel’s blog.
In any event, as the name suggests, such organizations would be provider-led and would be operated through a capitated system for managing the costs of the Medicaid program. The Senate bill would result in up to twelve PLEs being awarded contracts on a regional basis.
PLEs are not the only addition to the Medicaid alphabet soup that the Senate is proposing in its version of HB 372. The Senate has also renewed its interest in taking Medicaid out of the hands of the N.C. Department of Health and Human Services entirely and creating a new state agency, the Department of Medicaid (“DOM”).
(One wonders whether the continual interest in creating a new Department of Medicaid independent of the N.C. Department of Health and Human Services had anything to do with embattled DHHS Secretary Wos stepping down recently.)
The Senate also proposes creating a Joint Legislative Oversight Committee on Medicaid (“LOC on Medicaid”).
But creating the DOM and using new PLEs to handle the provision of Medicaid services is not the whole story. Perhaps unwilling to jump entirely into a new delivery system managed by a wholly new state agency, the Senate bill would keep LME/MCOs for mental health services in place for at least another five years. Private contractor MCOs would also operate alongside the PLEs. The North Carolina Medicaid Choice coalition, a group which represents commercial MCOs in connection with the Medicaid reform process, is pleased.
One very interesting item that the Senate has included in its proposed legislation is the following requirement: “Small providers shall have an equal opportunity to participate in the provider networks established by commercial insurers and PLEs, and commercial insurers and PLEs shall apply economic and quality standards equally regardless of provider size or ownership.” You can thank Senator Joel Ford of Mecklenburg County for having sponsored this amendment to the Senate version of House Bill 372.
By pulling the Medicaid reform proposal out of the budget bill, the matter appears headed for further negotiation between the House and the Senate to see if the two can agree this year, unlike last year.
By legislative standards, that counts as forward progress… Here come the legislative discussion committees to hash it out more between the two chambers. We will keep a close eye on the proposals as they continue to evolve.
By Robert Shaw

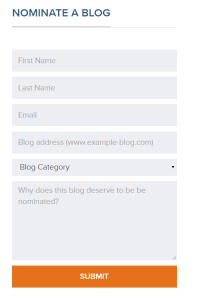
Consider Nominating This Blog for the 2015 Best Legal Blog Contest (Please)!
The 2015 Legal Blog Contest is here!
For all you that follow this blog, thank you! I hope that you agree that I provide you with valuable and up-to-date information on Medicaid/care regulatory issues. At least, that is my hope in maintaining this blog. And maintaining this blog takes a lot of time outside my normal, hectic legal career and my time as a mom and wife. Don’t get me wrong…I love blogging about these issues because these issues are near and dear to my heart. I am passionate about health care, health care providers, Medicaid and Medicare, and access to quality care.
If you are a follower, then you know that I try to keep my readers current on Medicaid/care fraud, federal and state laws, legal rights for health care providers, bills in the General Assembly germane to health care, extrapolation issues, CMS rulings, managed care matters, reimbursement rates, RAC audits and much, much more!
If you enjoy my blog, I ask a favor. Please consider nominating my blog for the 2015 Best Legal Blog Contest.
If you want to nominate my blog, please click here.
Scroll down until you see this:
Enter your name, email address, my blog address. which is:
For category, click on “Niche and Specialty.” I do not believe the other categories correctly describe my blog.
And type a reason why you enjoy my blog. Much appreciated!

NC MCOs and Consolidation: “When the Music Stops? Nobody Knows!”
Our General Assembly is pushing for the managed care organizations (MCOs) to consolidate and/or morph. Consolidating the MCOs makes fiscal sense for our state, but if I were executive management at an MCO, I would be be anxiously awaiting direction from our General Assembly. A metaphoric 3-4 chair game of”Musical Chairs” is proceeding with 9 (now 8) players. Five to six players will have no chairs when the music stops.
What are MCOs? See blog and blog.
Multiple bills have been proposed.
Senate Bill 703 proposes 3 statewide MCOs. Senate Bill 574 seems to incorporate provider-led capitated health plans, but is unclear as to the exact model. Senate Bill 696 seems to create a symphony of provider-led and nonprovider-led, risk-based entities. Senate Bill 568 contemplates licensed commercial health insurers offering health care plans.
No one really knows how many MCOs will remain in the end…if any. Regardless, what the number of existing MCOs in the future will be, there is little dispute that the number will be fewer than the number of MCOs that exist now.
In an atmosphere where there is supposition that there are too many people or companies and that only a few will remain, competition brews. People/companies are forced to strategize if they want to survive.
Think about the childhood game, “Musical Chairs.” You start with a large group of people, but with one less chair than the number of people. The music plays and the players meander around at a relatively slow pace, around and around, until the music stops. And what happens when the music stops? The people scramble for a chair. The person left standing is “out” and must sit on the sideline.
We have 9, soon to be 8, MCOs in NC right now. And the music is playing. But which MCOs will be left standing when the music stops?
Here is a map of our current MCOs:
As of July 1, CoastalCare and East Carolina Behavioral Healthcare (ECBH) will be merged. We will be down to 8 MCOs. Which means that the light blue on the bottom right hand side of the map will merge with the bright yellow on top right hand side of the map.
Mecklenburg county, which houses most of the Charlotte area, was not always light purple. It recently merged with Cardinal Innovations.
Partners (light yellow) and Smokey Mountain (dark blue) had serious discussions of a merger until, recently, when both walked away from negotiations of merger.
Why should it matter which MCOs are in existence or how many? Theoretically, it shouldn’t. These MCOs are created in order to manage behavioral health care (Medicaid services for those suffering from substance abuse, mental illness, and developmentally disabled), not to make a profit, right? The only issue of importance should be that medically necessary behavioral health care services are rendered to Medicaid recipients in the most efficient and most effective manner.
Yet competing interests come into play.
Think about it…each MCO employs hundreds of people. Each MCO has a CEO, who is not working for free. Generally, unless other arrangements have been negotiated, there can only be one CEO per MCO. When there are 2+ MCOs merging with 2 CEOs and only 1 “chair” for 1 CEO, it can seem like “Musical Chairs.” Multiple people are vying for one “chair.”
The money at issue for behavioral health care in NC is not a small amount. It is likened to a fire hose spouting money. We have a Medicaid budget in NC of approximately 14 billion dollars. To put it in perspective, with $14 billion dollars, you could purchase the LA Lakers 14 times. This is how much money we spend on Medicaid every year. It is really quite staggering when you think about it.
As every North Carolinian learns in the 6th grade, North Carolina is composed of 100 counties. The estimated Medicaid budget of $14 billion is allocated across 100 counties and among approximately 1.9 million Medicaid recipients.
When it was decided to implement the MCOs across the state, about 2012-ish (we actually obtained permission from CMS for the waiver years prior to 2012, but we began with a pilot and did not implement the MCOs statewide until 2012-13), we found ourselves, initially, with eleven MCOs, and now we have 9…soon to be 8.
The newly merged entity of CoastalCare and ECBH (CC+ECBH) will manage state funds and Medicaid dollars for behavioral health services across 24 counties in eastern North Carolina. In other words almost ¼ of the Medicaid budget will be handed to CC+ECBH, leaving approximately ¾ of the Medicaid budget for 7 other MCOs (the budget is determined by number of recipients, so I am assuming, for the purpose of this blog, that more counties mean more people).
The amount of counties controlled by the remaining 7 MCOs are as follows:
Smokey: 23
Partners: 8
Centerpointe: 4
Cardinal: 16
Sandhills: 9
Eastpointe: 12
Alliance: 4
Looking at the chart above, it would appear that Smoky and CC+ECBH will manage almost 1/2 the state’s behavioral health care for Medicaid.
Prior to the 1915 b/c Waiver allowing the MCOs to manage behavioral services for Medicaid recipients in NC, DHHS managed it. (Obviously ValueOptions and other vendors had a part in it, but not with actual management). As the single state agency for Medicaid, DHHS cannot delegate administrative duties to contracted parties without a “Waiver,” or permission for an exception from the federal government, or, more specifically, the Center for Medicare and Medicaid Services (CMS).
Prior to the 1915 b/c Waiver, we did not have 9 companies with hundreds of employees managing behavioral health care for Medicaid recipients. We had DHHS, which employs approximately 18,000 employees. To my knowledge DHHS did not terminate those employees who were in charge of behavioral health care issues in order to compensate the creation of new companies/employees. In other words, say 1000 people at DHHS devoted their time to issues arising our of behavioral health care. Once we had an additional 9 (well, 11, at first), those 1000 employees were not asked to join the MCOs. Maybe some did, but, to my knowledge, there was no suggestion or incentive or requirement to leave DHHS and go to an MCO (to shift the administrative burden).
When we created an additional 9 (well, 11 at first) companies to, essentially, take over behavioral health care…
We created more administrative costs, in order to lift the risk of overspending the Medicaid budget off the state. It is estimated that America wastes $190 billion in excess administrative costs per year.
In theory, consolidating the MCOs would decrease administrative costs by having fewer paid employees, not dissimilar to why MCOs want a closed network. See blog. Again, in theory, having fewer MCOs may create a more consistent statewide manner in managing behavioral health care.
Assume for the purpose of this blog that each MCO employs 100 people (which is a very low number) and each employee is paid $50,000, then the administrative cost associated with delegating behavioral health care to MCOs equals $500,000, counting only employee salaries. Multiple that number by 9 (number of current MCOs) and you get an increased administrative cost of approximately $4.5 million dollars per year, not counting the additional overhead each MCO bears (rent/mortgage, equipment, salary benefits, health care benefits, etc.). Plus you have to include the top management’s salaries, because you know the executives are receiving more than $50,000/year.
What motivated us to implement a MCOs system? With an MCO system, the General Assembly is able to allocate funds for Medicaid and place the risk of going over the budget on the MCOs, not the state. This is a completely understandable and reasonable objective. It is without question that the Medicaid budget is swelling to the point of unsustainability.
However, are we trading “control/supervision” for “knowability?” Are we also trading “risk” for “higher administrative costs,” which, in turn, equals less Medicaid dollars for providers and Medicaid recipients? Every dollar paid to an MCO employee is a dollar not going to a health care provider to reimburse for services.
For these reasons, the government’s push for consolidation of the MCOs is astute. Fewer MCOs = less administrative costs. Fewer MCOs = easier supervision by DHHS.
Less administrative costs = more Medicaid dollars going to providers…to serve our most needy. Because, at the end of the day, the most important issue when it comes to Medicaid is providing quality care for recipients.
It is no matter which entity controls/manages behavioral health care for Medicaid, because regardless the entity, that entity should be managing our tax dollars in the most efficient way that provides the best quality to services to those in need.
“Around and around we go, when we stop? Nobody knows…” But we do know this…when the music stops, there will be scrambling!
New NC Senate Bill Proposes 4-6 MCOs!! And the Creation of ARPLOs!!
Senate Bill 568 was filed today!!! It is a bill that you should follow!
SB 568 reads: “It is the intent of the General Assembly to transform the State’s health care purchasing methods from a traditional fee-for-service system into a value-based system that provides budget predictability for the taxpayers of this State while ensuring quality care to those in need.”
It proposes, among other things, a consolidation of the 9 current managed care organizations (MCO) here in North Carolina to “not more than 6” and “no less than 4” MCOs.
It further establishes another acronym: ARPLOs.
“At-Risk Provider-Led Organizations (ARPLOs). ARPLOs are capitated health plans administered by North Carolina’s provider-led Accountable Care Organizations that will manage and coordinate the care for the Patient Population, outside of the PCMHs, pending waiver approval where appropriate for this transformation by the Center for Medicare & Medicaid Services.”
Remember, the House has pushed for ACOs and the Senate has pushed for MCOs. See blog.
Is the Senate bending toward the House??????
More to come…