Blog Archives
House Bill 403: A Potential Upheaval of Medicaid!
Is this the end of the managed care organizations (MCOs)?
If the Senate’s proposed committee substitute (PCS) to House Bill 403 (HB 403) passes the answer is yes. The Senate’s PCS to House Bill 403 was just favorably reported out of the Senate Health Care Committee on June 15, 2017. The next step for the bill to advance will be approval by the Senate Rules Committee. Click here to watch its progress.
As my readers are well aware, I am not a proponent for the MCOs. I think the MCOs are run by overpaid executives, who pay themselves too high of bonuses, hire charter flights, throw fancy holiday parties, and send themselves and their families on expensive retreats – to the detriment of Medicaid recipients’ services and Medicaid providers’ reimbursement rates. See blog. And blog.
Over the last couple days, my email has been inundated by people abhorred with HB 403 – urging the Senators to retain the original HB 403, instead of the PCS version. As with all legislation, there are good and bad components. I went back and re-read these emails, and I realized multiple authors sat on an MCO Board. Of course MCO Board members will be against HB 403! Instead of hopping up and down “for” or “against” HB 403, I propose a (somewhat) objective review of the proposed legislation in this blog.
While I do not agree with everything found in HB 403, I certainly believe it is a step in the right direction. The MCOs have not been successful. Medically necessary behavioral health care services have been reduced or terminated, quality health care providers have been terminated from catchment areas, and our tax dollars have been misused.
However, I do have concern about how quickly the MCOs would be dissolved and the new PHPs would be put into effect. There is no real transition period, which could provide safety nets to ensure continuity of services. We all remember when NCTracks was implemented in 2013 and MMIS was removed on the same day. There was no overlap – and the results were catastrophic.
The following bullet points are the main issues found in HB 403, as currently written.
- Effective date – MCOs dissolve immediately (This could be dangerous if not done properly)
Past legislation enacted a transition time to dissolve the MCOs. Session Law 2015-245, as amended by Session Law 2016-121, provided that the MCOs would be dissolved in four years, allowing the State to implement a new system slowly instead of yanking the tablecloth from the table with hopes of the plates, glasses, and silverware not tumbling to the ground.
According to HB 403, “on the date when Medicaid capitated contracts with Prepaid Health Plans (PHPs) begin, as required by S.L. 2015-245, all of the following shall occur:…(2) The LME/MCOs shall be dissolved.”
Session Law 2015-245 states the following timeline: “LME/MCOs shall continue to manage the behavioral health services currently covered for their enrollees under all existing waivers, including the 1915(b) and (c) waivers, for four years after the date capitated PHP contracts begin. During this four-year period, the Division of Health Benefits shall continue to negotiate actuarially sound capitation rates directly
with the LME/MCOs in the same manner as currently utilized.”
HB 403 revises Session Law 2015-245’s timeline by the following: “LME/MCOs shall continue to manage the behavioral health services currently covered for their enrollees under all existing waivers, including the 1915(b) and (c) waivers, for four years after the date capitated PHP contracts begin. During this four-year period, the Division of Health Benefits shall continue to negotiate actuarially sound capitation rates directly with the LME/MCOs in the same manner as currently utilized.”
Instead of a 4-year transition period, the day the PHP contracts are effective, the MCOs no longer exist. Poof!! Maybe Edward Bulwer-Lytton was right when he stated, “The pen is mightier than the sword.”
Again, I am not opposed to dissolving the MCOs for behavioral health care; I just want whatever transition to be reasonable and safe for Medicaid recipients and providers.
With the MCOs erased from existence, what system will be put in place? According to HB 403, PHPs shall manage all behavioral health care now managed by MCOs and all the remaining assets (i.e., all those millions sitting in the savings accounts of the MCOs) will be transferred to DHHS in order to fund the contracts with the PHPs and any liabilities of the MCOs. (And what prevents or does not prevent an MCO simply saying, “Well, now we will act as a PHP?”).
What is a PHP? HB 403 defines PHPs as an entity, which may be a commercial plan or provider-led entity with a PHP license from the Department of Insurance and will operate a capitated contract for the delivery of services. “Services covered by PHP:
- Physical health services
- Prescription drugs
- Long-term care services
- Behavioral health services
The capitated contracts shall not cover:
Behavioral healthDentist services- The fabrication of eyeglasses…”
It would appear that dentists will also be managed by PHPs. As currently written, HB 403 also sets no less than three and no more than five contracts between DHHS and the PHPs should be implemented.
Don’t we need a Waiver from the Center for Medicare and Medicaid Services (CMS)?
Yes. We need a Waiver. 42 CFR 410.10(e) states that “[t]he Medicaid agency may not delegate, to other than its own officials, the authority to supervise the plan or to develop or issue policies, rules, and regulations on program matters.” In order to “Waive” this clause, we must get permission from CMS. We had to get permission from CMS when we created the MCO model. The same is true for a new PHP model.
Technically, HB 403 is mandating DHHS to implement a PHP model before we have permission from the federal government. HB 403 does instruct DHHS to submit a demonstration waiver application. Still, there is always concern and hesitancy surrounding implementation of a Medicaid program without the blessing of CMS.
- The provider network (This is awesome)
HB 403 requires that all contracts between PHPs and DHHS have a clause that requires PHPs to not exclude providers from their networks except for failure to meet objective quality standards or refusal to accept network rates.
- PHPs use of money (Also good)
Clearly, the General Assembly drafted HB 403 out of anger toward the MCOs. HB 403 implements more supervision over the new entities. It also disallows use of money on alcohol, first-class airfare, charter flights, holiday parties or similar social gatherings, and retreats, which, we all know these are precisely the activities that State Auditor Beth Wood found occurring, at least, at Cardinal. See Audit Report.
HB 403 also mandates that the Office of State Human Resources revise and update the job descriptions for the area directors and set limitations on salaries. No more “$1.2 million in CEO salaries paid without proper authorization.”
- Provider contracts with the PHPs (No choice is never good)
It appears that HB 403 will not allow providers to choose which PHP to join. DHHS is to create the regions for the PHPs and every county must be assigned to a PHP. Depending on how these PHPs are created, we could be looking at a similar situation that we have now with the MCOs. If the State is going to force you to contract with a PHP to provide Medicaid services, I would want the ability to choose the PHP.
In conclusion, HB 403 will re-shape our entire Medicaid program, if passed. It will abolish the MCO system, apply to almost all Medicaid services (both physical and mental), open the provider network, limit spending on inappropriate items, and assign counties to a PHP.
Boy, what I would give to be a fly on the wall in all the MCO’s boardrooms (during the closed sessions).
Another Win! 12 Million Dollar Recoupment Reduced to $896 – But There is a Twist
One of our clients in New Mexico had an alleged Medicaid recoupment of over $12 million!! Actually, $12,015,850.00 – to be exact. (See below). After we presented our evidence and testimony, the Judge found that we owe $896.35. I call that a win!
In this case, the Human Services Department (HSD) in New Mexico had reviewed 150 random claims. Initially, HSD claimed that 41 claims out of 150 were noncompliant.

But, prior to the hearing, we saved over $10 million by pointing out HSD’s errors and/or by providing additional documentation.
And then the ALJ’s decision after we presented our evidence and testimony –

Boom! Drop the mike…
…………………………….not so fast…
……………………………………………..picking the mike back up…
You see, in New Mexico, the administrative law judges (ALJs) cannot render decisions. Look in the above picture. You see where it reads, “Recommendation?” That is because the ALJs in New Mexico can only render recommendations.
Because Medicaid has a “single state agency” rule; i.e., that only one agency may render discretionary decisions regarding Medicaid, and HSD is the single state agency in New Mexico charged with managing Medicaid, only HSD may render a discretionary decision. So in NM, the ALJ makes a recommendation and then the Secretary of HSD has the choice to either accept or reject the decision.
Guess whether HSD accepted or rejected the ALJ’s recommendation?

Now we will have to appeal the Agency’s Decision to overturn the ALJ recommendation.
Here, in NC, we obtained a waiver from the Centers of Medicare and Medicaid Services (CMS) to allow our ALJs to render Decisions. See blog.
I still consider this a win.
Medicaid Closed Networks: Can Waivers Waive Your Legal Rights?
Sorry for the lapse in blogging. I took off for Thanksgiving and then got sick. I hope you all had a wonderful Thanksgiving!!
While I was sick, I thought about all the health care providers that have been put out of business because the managed care organization (MCO) in their area terminated their Medicaid contract or refused to contract with them. I thought about how upset I would be if I could not see my doctor, whom I have seen for years. See blog for “You Do Have Rights!”
Then I thought about…Can a Waiver waive a legal right?
Federal law mandates that Medicaid recipients be able to choose their providers of choice. Court have also held that this “freedom of choice” of provider is a right, not a privilege.
42 U.S.C. § 1396a states that Medicaid recipients may obtain medical services from “any institution, agency, community pharmacy, or person, qualified to perform the service or services required… who undertakes to provide him such services….” Id. at (a)(23).
So how can these MCOs restrict access?
First, we need to discuss the difference between a right and a privilege.
For example, driving is a privilege, not a right. You have no right to a driver’s license, which is why you can lose your license for things, such as multiple DUIs. Plus, you cannot receive a driver’s license unless you pass a test, because a license is not a right.
Conversely, you have the right to free speech and the right to vote. Meaning, the government cannot infringe on your rights to speak and vote unless there are extraordinary circumstances. For example, the First Amendment does not protect obscenity, child pornography, true threats, fighting words, incitement to imminent lawless action (yelling “fire” in a crowded theater), criminal solicitation or defamation. Your right to vote will be rescinded if you are convicted of a felony. Furthermore, you do not need to take a test or qualify for the rights of free speech and voting.
Likewise, your choice of health care provider is a right. It can only be usurped in extraordinary circumstances. You do not need to take a test or qualify for the right. (Ok, I am going to stop underlining “right” and “privilege” now. You get the point).
Then how are MCOs operating closed networks? For that matter, how can Blue Cross Blue Shield (BCBS) terminate a provider’s contract? Wouldn’t both those actions limit your right to choose your provider?
The answer is yes.
And the answer is simple for BCBS. As for BCBS, it is a private company and does not have to follow all the intricate regulations for Medicare/caid. 42 U.S.C. § 1396a is inapplicable to it.
But Medicaid recipients have the right to choose their provider. This “freedom of choice” provision has been interpreted by both the Supreme Court and the Seventh Circuit as giving Medicaid recipients the right to choose among a range of qualified providers, without government interference (or its agents thereof).
What does this mean? How can a managed care organization (MCO) here in NC maintain a closed network of providers without violating the freedom of choice of provider rule?
The “Stepford” answer is that we have our Waivers in NC, which have waived the freedom of choice. In our 1915 b/c Waiver, there are a couple pages that enumerates certain statutes. We “x” out the statutes that we were requesting to waive.
It looks like this:

Furthermore, federal law carves out an exception to freedom to choose right when it comes to managed care. But to what extent? It the federal carve unconstitutional?
But…the question is twofold:
- Would our Waiver stand up to federal court scrutiny?
- Can our state government waive your rights? (I couldn’t help it).
Let’s think of this in the context of the freedom of speech. Could NC request from the federal government a waiver of our right to free speech? It sounds ludicrous, doesn’t it? What is the difference between your right to free speech and your right to choose a provider? Is one right more important than the other?
The answer is that no one has legally challenged our Waiver’s waiver of the right to freedom of provider with a federal lawsuit claiming a violation of a constitutionally protected right. It could be successful. If so, in my opinion, two legal theories should be used.
- A § 1983 action; and/or
- A challenge under 42 CFR 431.55(f)
Section 1983 creates a federal remedy against anyone who deprives “any citizen of the United States… of any rights, privileges, or immunities secured by the Constitution and laws” under the color of state law. 42 U.S.C. § 1983. The Supreme Court has explained that § 1983 should be read to generally “authorize[] suits to enforce individual rights under federal statutes as well as the Constitution.” City of Rancho Palos Verdes, Cal. v. Abrams, 544 U.S. 113, 119 (2005).
Section 1983 does not authorize a federal remedy against state interference with all government entitlements, however; “it is rights, not the broader or vaguer ‘benefits’ or ‘interests,’ that may be enforced under the authority of that section.” Gonzaga Univ. v. Doe, 536 U.S. 273, 283 (2002). But the courts have already held that the freedom to choose your provider is a right.
In 2012, the Seventh Circuit confirmed that § 1983 authorizes Medicaid recipients to sue to enforce the right to freely choose among qualified health providers.
In Planned Parenthood, the court was confronted with an Indiana state law prohibiting state agencies from providing state or federal funds to any entity that performs abortions or maintains or operates a facility in which abortions are performed – regardless of whether there is any nexus between those funds and the abortion services. See Planned Parenthood, 699 F.3d at 967 (7th Cir. 2012). In other words, the law effectively prohibited entities that perform abortions from receiving any state or federal funds for any (non-abortion) purpose.
The Court found that the restrictions violated the Medicaid recipients’ right to freedom of choice of provider.
There are, as always, more than one way to skin a cat. You could also attack the Waiver’s waiver of the freedom to choose your health care provider by saying the NC is violating 42 CFR 431.55.
Notice the last sentence in subsection (d) in the picture above. In our Waiver, NC promises to abide by 42 CFR 431.55(f), which states:
Basically, to argue a violation of 42 CFR 431.55, you would have to demonstrate that NC violated or is violating the above regulation by not providing services “consistent with access, quality and efficient and economic provision of covered care and services.”
So, while it is true that NC has requested and received permission from the Center of Medicare and Medicaid Services (CMS) to restrict access to providers, that fact may not be constitutional.
Someone just needs to challenge the Waiver’s waiver.
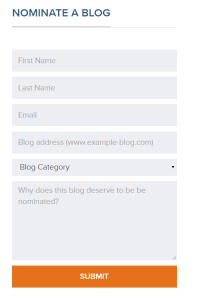
Consider Nominating This Blog for the 2015 Best Legal Blog Contest (Please)!
The 2015 Legal Blog Contest is here!
For all you that follow this blog, thank you! I hope that you agree that I provide you with valuable and up-to-date information on Medicaid/care regulatory issues. At least, that is my hope in maintaining this blog. And maintaining this blog takes a lot of time outside my normal, hectic legal career and my time as a mom and wife. Don’t get me wrong…I love blogging about these issues because these issues are near and dear to my heart. I am passionate about health care, health care providers, Medicaid and Medicare, and access to quality care.
If you are a follower, then you know that I try to keep my readers current on Medicaid/care fraud, federal and state laws, legal rights for health care providers, bills in the General Assembly germane to health care, extrapolation issues, CMS rulings, managed care matters, reimbursement rates, RAC audits and much, much more!
If you enjoy my blog, I ask a favor. Please consider nominating my blog for the 2015 Best Legal Blog Contest.
If you want to nominate my blog, please click here.
Scroll down until you see this:
Enter your name, email address, my blog address. which is:
For category, click on “Niche and Specialty.” I do not believe the other categories correctly describe my blog.
And type a reason why you enjoy my blog. Much appreciated!

NC MCOs and Consolidation: “When the Music Stops? Nobody Knows!”
Our General Assembly is pushing for the managed care organizations (MCOs) to consolidate and/or morph. Consolidating the MCOs makes fiscal sense for our state, but if I were executive management at an MCO, I would be be anxiously awaiting direction from our General Assembly. A metaphoric 3-4 chair game of”Musical Chairs” is proceeding with 9 (now 8) players. Five to six players will have no chairs when the music stops.
What are MCOs? See blog and blog.
Multiple bills have been proposed.
Senate Bill 703 proposes 3 statewide MCOs. Senate Bill 574 seems to incorporate provider-led capitated health plans, but is unclear as to the exact model. Senate Bill 696 seems to create a symphony of provider-led and nonprovider-led, risk-based entities. Senate Bill 568 contemplates licensed commercial health insurers offering health care plans.
No one really knows how many MCOs will remain in the end…if any. Regardless, what the number of existing MCOs in the future will be, there is little dispute that the number will be fewer than the number of MCOs that exist now.
In an atmosphere where there is supposition that there are too many people or companies and that only a few will remain, competition brews. People/companies are forced to strategize if they want to survive.
Think about the childhood game, “Musical Chairs.” You start with a large group of people, but with one less chair than the number of people. The music plays and the players meander around at a relatively slow pace, around and around, until the music stops. And what happens when the music stops? The people scramble for a chair. The person left standing is “out” and must sit on the sideline.
We have 9, soon to be 8, MCOs in NC right now. And the music is playing. But which MCOs will be left standing when the music stops?
Here is a map of our current MCOs:
As of July 1, CoastalCare and East Carolina Behavioral Healthcare (ECBH) will be merged. We will be down to 8 MCOs. Which means that the light blue on the bottom right hand side of the map will merge with the bright yellow on top right hand side of the map.
Mecklenburg county, which houses most of the Charlotte area, was not always light purple. It recently merged with Cardinal Innovations.
Partners (light yellow) and Smokey Mountain (dark blue) had serious discussions of a merger until, recently, when both walked away from negotiations of merger.
Why should it matter which MCOs are in existence or how many? Theoretically, it shouldn’t. These MCOs are created in order to manage behavioral health care (Medicaid services for those suffering from substance abuse, mental illness, and developmentally disabled), not to make a profit, right? The only issue of importance should be that medically necessary behavioral health care services are rendered to Medicaid recipients in the most efficient and most effective manner.
Yet competing interests come into play.
Think about it…each MCO employs hundreds of people. Each MCO has a CEO, who is not working for free. Generally, unless other arrangements have been negotiated, there can only be one CEO per MCO. When there are 2+ MCOs merging with 2 CEOs and only 1 “chair” for 1 CEO, it can seem like “Musical Chairs.” Multiple people are vying for one “chair.”
The money at issue for behavioral health care in NC is not a small amount. It is likened to a fire hose spouting money. We have a Medicaid budget in NC of approximately 14 billion dollars. To put it in perspective, with $14 billion dollars, you could purchase the LA Lakers 14 times. This is how much money we spend on Medicaid every year. It is really quite staggering when you think about it.
As every North Carolinian learns in the 6th grade, North Carolina is composed of 100 counties. The estimated Medicaid budget of $14 billion is allocated across 100 counties and among approximately 1.9 million Medicaid recipients.
When it was decided to implement the MCOs across the state, about 2012-ish (we actually obtained permission from CMS for the waiver years prior to 2012, but we began with a pilot and did not implement the MCOs statewide until 2012-13), we found ourselves, initially, with eleven MCOs, and now we have 9…soon to be 8.
The newly merged entity of CoastalCare and ECBH (CC+ECBH) will manage state funds and Medicaid dollars for behavioral health services across 24 counties in eastern North Carolina. In other words almost ¼ of the Medicaid budget will be handed to CC+ECBH, leaving approximately ¾ of the Medicaid budget for 7 other MCOs (the budget is determined by number of recipients, so I am assuming, for the purpose of this blog, that more counties mean more people).
The amount of counties controlled by the remaining 7 MCOs are as follows:
Smokey: 23
Partners: 8
Centerpointe: 4
Cardinal: 16
Sandhills: 9
Eastpointe: 12
Alliance: 4
Looking at the chart above, it would appear that Smoky and CC+ECBH will manage almost 1/2 the state’s behavioral health care for Medicaid.
Prior to the 1915 b/c Waiver allowing the MCOs to manage behavioral services for Medicaid recipients in NC, DHHS managed it. (Obviously ValueOptions and other vendors had a part in it, but not with actual management). As the single state agency for Medicaid, DHHS cannot delegate administrative duties to contracted parties without a “Waiver,” or permission for an exception from the federal government, or, more specifically, the Center for Medicare and Medicaid Services (CMS).
Prior to the 1915 b/c Waiver, we did not have 9 companies with hundreds of employees managing behavioral health care for Medicaid recipients. We had DHHS, which employs approximately 18,000 employees. To my knowledge DHHS did not terminate those employees who were in charge of behavioral health care issues in order to compensate the creation of new companies/employees. In other words, say 1000 people at DHHS devoted their time to issues arising our of behavioral health care. Once we had an additional 9 (well, 11, at first), those 1000 employees were not asked to join the MCOs. Maybe some did, but, to my knowledge, there was no suggestion or incentive or requirement to leave DHHS and go to an MCO (to shift the administrative burden).
When we created an additional 9 (well, 11 at first) companies to, essentially, take over behavioral health care…
We created more administrative costs, in order to lift the risk of overspending the Medicaid budget off the state. It is estimated that America wastes $190 billion in excess administrative costs per year.
In theory, consolidating the MCOs would decrease administrative costs by having fewer paid employees, not dissimilar to why MCOs want a closed network. See blog. Again, in theory, having fewer MCOs may create a more consistent statewide manner in managing behavioral health care.
Assume for the purpose of this blog that each MCO employs 100 people (which is a very low number) and each employee is paid $50,000, then the administrative cost associated with delegating behavioral health care to MCOs equals $500,000, counting only employee salaries. Multiple that number by 9 (number of current MCOs) and you get an increased administrative cost of approximately $4.5 million dollars per year, not counting the additional overhead each MCO bears (rent/mortgage, equipment, salary benefits, health care benefits, etc.). Plus you have to include the top management’s salaries, because you know the executives are receiving more than $50,000/year.
What motivated us to implement a MCOs system? With an MCO system, the General Assembly is able to allocate funds for Medicaid and place the risk of going over the budget on the MCOs, not the state. This is a completely understandable and reasonable objective. It is without question that the Medicaid budget is swelling to the point of unsustainability.
However, are we trading “control/supervision” for “knowability?” Are we also trading “risk” for “higher administrative costs,” which, in turn, equals less Medicaid dollars for providers and Medicaid recipients? Every dollar paid to an MCO employee is a dollar not going to a health care provider to reimburse for services.
For these reasons, the government’s push for consolidation of the MCOs is astute. Fewer MCOs = less administrative costs. Fewer MCOs = easier supervision by DHHS.
Less administrative costs = more Medicaid dollars going to providers…to serve our most needy. Because, at the end of the day, the most important issue when it comes to Medicaid is providing quality care for recipients.
It is no matter which entity controls/manages behavioral health care for Medicaid, because regardless the entity, that entity should be managing our tax dollars in the most efficient way that provides the best quality to services to those in need.
“Around and around we go, when we stop? Nobody knows…” But we do know this…when the music stops, there will be scrambling!
Broken Promises and the NC Waiver: You Do NOT Get Your Choice of Provider!!
In the 1968 Presidential campaign, Richard Nixon stated that “new leadership will end the war” in Vietnam. Also, in a 1968 interview, Nixon said he had “no magic formula” or “gimmick” for ending the Vietnam War. Then, in his memoirs, Nixon stated he never claimed to have such a plan. This is called a broken election promise.
Sadly, Richard Nixon’s broken election promise was not the first, nor would it be the last. We have become used to politicians making election promises and breaking those same promises which got them elected once they are in office.
“If you like your doctor, you can keep your doctor. If you like your health care plan, you can keep your health care plan.”
“Read my lips: no new taxes.”
Over the last few years, I have written ad nausem about accountability and proper supervision when it comes to the Managed Care Organizations (MCOs) in North Carolina. The other day, I was reviewing some pertinent federal regulations and came across this:
§ 438.52 Choice of MCOs, PIHPs, PAHPs, and PCCMs.
• General rule. Except as specified in paragraphs (b) and (c) of this section, a State that requires Medicaid beneficiaries to enroll in an MCO, PIHP, PAHP, or PCCM must give those beneficiaries a choice of at least two entities.
Obviously, North Carolina is not adhering to the above-referenced requirement.
Pull up the Waiver. In order to offer Medicaid enrollees only one MCO or other such entity, North Carolina would have had to request a waiver of 42 CFR § 438.52.If you rely on Medicaid for behavioral health care and live in Wake County, you have no choice but to rely on the provider network of only entity, Alliance Behavioral Health (Alliance), to receive services. For example, you do not get to choose between Alliance’s provider network and Eastpointe Behavioral Healthcare’s (Eastpointe) provider network. Staying with the same theoretical hypothesis, if your provider was not anointed with the gift of being in Alliance’s network, then you do not get to stay with your provider.
“If you like your doctor, you can keep your doctor. If you like your health care plan, you can keep your health care plan.”
Similar to President Barack Obama’s contention quoted above, we made similar promises to the Center for Medicare and Medicaid Services (CMS). Our promises are found within our Waivers. We have two Waivers, one for the developmentally disabled population and one for the mentally ill/substance abuse population. Each Waiver waives certain federal exceptions. However, in lieu of the federal requirements, we make certain promises to CMS. In order to waive 42 CFR § 438.52, we made certain promises to CMS in order to circumvent the necessary provisions of 42 CFR § 438.52.
The State sought a waiver of section 1902(a)(4) of the Act:
“The State seeks a waiver of section 1902(a)(4) of the Act, which requires States to offer a choice of more than one PIHP or PAHP per 42 CFR 438.52. Please describe how the State will ensure this lack of choice of PIHP or PAHP is not detrimental to beneficiaries’ ability to access services.”
Here are our promises:
“Under these circumstances, the State does not believe that making only one plan available in each geographic area of the State will negatively impact recipients’ access to care.”
“The LMEs have decades of experience locating and developing services for consumers with MH/IDD/SAS needs, and over the years, have built strong and collaborative working relationships with the providers of these services.”
“These providers support this initiative and consumers have at least as much choice in individual providers as they had in the non-managed care environment.”
“Enrollees will have free choice of providers within the PIHP serving their respective geographic area and may change providers as often as desired. If an individual joins the PIHP and is already established with a provider who is not a member of the network, the PIHP will make every effort to arrange for the consumer to continue with the same provider if the consumer so desires.”
“If you like your doctor, you can keep your doctor. If you like your health care plan, you can keep your health care plan.”
My two personal favorites among the State’s promises to CMS are: (1) “consumers have at least as much choice in individual providers as they had in the non-managed care environment;” and (2) the PIHP will make every effort to arrange for the consumer to continue with the same provider if the consumer so desires.”
These promises, in reality, are utter horsefeathers.
Over and over my provider clients come to me because one of the MCOs has terminated their Medicaid contract, usually for absolutely no valid reason. Over and over my provider clients tell me that their consumers are devastated by the news that they may lose their provider. I have had consumers contact me to beg me to help the provider. I have had consumers appear in court stating how much they want that particular provider. I have had provider clients cry in my office because their consumers are so upset and regressing because of the news that they may have to find another provider.
Yet, we have promised CMS that consumers have just as much choice in providers than when there was no managed care.
In the words of Dorothy from the Wizard of OZ, “You ought to be ashamed of yourself. Frightening him like that when he came to you for help.”
Similarly, our Medicaid recipients go to their providers for help. They create relationships…trust…bonds. And the MCOs are terminating these very providers, most for invalid and erroneous reasons, and, certainly, without the consideration of our promise to CMS.
But, remember, we are told the PIHPs will make every effort to keep the consumer with the chosen provider…
It would be interesting to do a public records request as to how many providers have been terminated by the MCOs in the last 2 years. Because, even if only 1 provider were terminated in the past 2 years and its consumers still wanted to go to that particular provider, then our State has broken its promise.
Apparently, due to my outspoken positions, DHHS will no longer honor my public records requests, which I think is absolutely preposterous. I am, still, a paying taxpayer last time I checked, which is every pay-day when I only get 60% of my wages. If any of you would submit this public records request, please forward it to me. I would be grateful for the information.
Williams Mullen Hosts “The State of the State of Health Care” Panel Discussion
Williams Mullen is hosting a free panel discussion on “The State of the State of Health Care.” Please see below!
The panelists will be Rep. Nelson Dollar, Steven Keene, General Counsel to the NC Medical Society, Barbara Burke, from BCBS, and me. The panel discussion will begin at 4:00. Then from 5:00-6:30 we will have free drinks and appetizers.
Please feel free to come and bring others. But we do request that you register here by October 10th in order for us to have a correct head count.
Personal Care Services: Will the Fear of the “F” Word (Medicaid Fraud) Cause PCS in the Home to Be Eradicated???
In my career, I call it the “F” word:
Fraud.
Its existence and fear of existence drives Medicare and Medicaid policies.
It is without question that Medicare and Medicaid fraud needs to be eliminated. In fact, for true Medicare and Medicaid fraud, I propose harsher penalties. Think about what the fraudulent provider is doing…taking health care dollars from the elderly and poor without providing services. Medicare and Medicaid recipients receive less medically necessary services because of fraudulent providers.
Just recently, in Charlotte, on April 9, 2014, V.F. Brewton, of Shelby, N.C., was sentenced to 111 months in prison, three years of supervised release and ordered to pay $7,070,426 in restitution to Medicaid and $573,392 to IRS. On April 8, 2014, co-defendant, R. S. Cannon, of Charlotte, was sentenced to 102 months in prison, three years court supervised release and ordered to pay $2,541,306 in restitution. See press release. Ouch!
On November 21, 2013, in Miami, Fla., Roberto Marrero, who ran Trust Care, was sentenced 120 months in prison. From approximately March 2007 through at least October 2010, Trust Care submitted more than $20 million in claims for home health services. Medicare paid Trust Care more than $15 million for these fraudulent claims. Marrero and his co-conspirators have also acknowledged their involvement in similar fraudulent schemes at several other Miami health care agencies with estimated total losses of approximately $50 million. See article. Ouch!
However, there are never the stories in the newspapers and media about all the services actually rendered to Medicare and Medicaid recipients by upstanding providers who do not commit fraud, but, instead, work very hard every day to stay up-to-date on regulations and policies and who do not reap much profit for the services provided. I guess that doesn’t make good journalism.
I recently attended the Association for Home and Hospice Care (AHHC) conference in RTP, NC. I met wonderful and non-fraudulent providers. Each provider I met was passionate and compassionate about their job. The only time money was brought up was to discuss the low reimbursement rates and the low profit margin for these providers.
In fact, one of the speakers even opined that, because of the alleged prevalence of fraud in home health care, the federal and state governments will continue to cut reimbursement rates for home health and hospice until over 50% of the agencies operate at a loss by 2017. That is a dismal thought! What happened to our right to pursue a career without intervention?
One provider informed me that, upon his or her information and belief, there is a chance that PCS, which is an optional program under Medicaid, may be wiped out in the near future by the General Assembly (PCS for home health and assisted living facilities, not the recipients covered by the Waiver).
What are personal care services (PCS)?
In the world of Medicaid and Medicare, there are a number of different types of PCS. No, actually, I think it is more apropos to say there are a number of different PCS recipients in the world of Medicaid and Medicare.
First, the definition/eligibility requirements:
Personal Care Services (PCS) are available to individuals who have a medical condition, disability, or cognitive impairment and demonstrate unmet needs for, at a minimum three of the five qualifying activities of daily living (ADLs) with limited hands-on assistance; two ADLs, one of which requires extensive assistance; or two ADLs, one of which requires assistance at the full dependence level. The five qualifying ADLs are eating, dressing, bathing, toileting, and mobility. See DMA website.
PCS are provided to developmentally disabled people under the 1915 b/c Waivers, people who reside in nursing homes and long-term assisted living facilities, and people who qualify to receive PCS in their homes. For purposes of this blog, I am writing about the latter three types of recipients. All 50 states allow PCS for qualified individuals, but the qualifications differ among the states.
In this day and age, the “F” word drives Medicaid and Medicare policies. Without question Medicaid fraud exists. Whether Medicaid fraud is as prevalent as some may believe, I am not sure. I have certainly witnessed honest providers accused of Medicaid fraud.
And home health care providers are viewed by some, generally, as the providers who can most easily commit Medicaid fraud (with which I do not agree, but must concede that home health care is more difficult to monitor). For example, a home health care provider goes to a person’s home and provides services. Who would know whether the home health care provider was billing for services on days he or she did not go to the recipient’s house? Not the recipient, because the recipient has no idea for what dates the provider is billing. Unlike an assisted living facility or nursing home that is easier to monitor and would have the documentation to show that the recipient actually lived in the facility.
Because of the alleged prevalence of fraud in home health care, apparently, (and with no independent verification on my part) some in North Carolina are questioning whether we should continue to reimburse PCS with Medicaid dollars, particularly as to home health. But if we stopped reimbursing for PCS in the homes, what would be the alternative? How would it affect North Carolinians? Would eliminating PCS save tax dollar money? Stop fraud?
When we evaluate the effects of whether to continue to reimburse for PCS with Medicaid dollars, we aren’t only talking about those served by PCS, but also the companies and all employees providing the home health. In 2012 in NC, approximately 40,000 were employed in home health.
Why is home health care important (or is it?)? Should we allow the “F” word to erase PCS in home health?
What is the alternative to home health? Answer: (1) Assisted living facilities? (2) Nursing homes? (3) A dedicated, family caregiver? (4) Nothing?
While there are, I am sure, many reasons that PCS in home health care is vital to our community, for the purposes of this blog, I am going to concentrate on cost savings to the taxpayers. Home health costs us (taxpayers) less money than other alternatives to home health.
Also, understand please that I am not advocating that everyone should receive home health instead of entering nursing homes or assisted living facilities. Quite the contrary, as both nursing homes and assisted living facilities are essential to NC. I am merely pointing out that all the services (home health, nursing homes, and assisted living facilities) are important.
What is the difference between assisted living and nursing homes?
An assisted living community provides communal living, usually with social activities, a cafeteria, laundry service, etc. I always think of my grandma at Glenaire in Cary, NC. She plays bridge, attends a book club, and even takes a computer course! She actually joined Facebook a couple of years ago!
A nursing home, on the other hand, provides 24-hour supervision by a licensed or registered nursing staff. Generally, the folks eligible to be admitted into an assisted living facility will be eligible to receive PCS (see the above definition/eligibility requirements). So, logically, the clientele in an assisted living facility receiving PCS could, in some cases, also be eligible to receive PCS in their home. Obviously a number of factors come into play to determine whether a person goes into an assisted living facility versus staying at home and receiving home health care: eligibility, family issues, money, condition of your home, money, desire for independence, money, health issues, and money.
Because of the level of supervision and skill required in a nursing home, a nursing home will be much more expensive than an assisted living facility. Insomuch as the assisted living facility will be less expensive than a nursing home, home health care, because you are paying for your own room and board, will be cheaper than both.
The average national cost for an assisted living facility in 2012 was $3,550/month. That’s $42,600/year. The average cost for an assisted living facility in 2012 in NC was $2900/month.
The average cost for a nursing home in NC for a semi-private room is $73,913 and $82,125 for a private room. That’s $225/day for a private room. For that price, you could get a room at a Ritz Carlton! (albeit not in a touristy area).
You think nursing homes are expensive in NC? Don’t move to NY!! In NY, for a semi-private room it costs $124,100/year and $130,670/year for a private room ($358/day!). Florida is a bit more expensive that NC too. In Florida, on average, a semi-private room in a nursing home costs $83,950 and a private room is approximately $91,615.
On the flip side, the average cost for a homemaker is $38,896. A home health aide costs, on average, $40,040.
If, in fact, NC ceases to reimburse PCS in home health, many of the people residing in their homes and relying on Medicaid-covered PCS will be forced to leave their homes for, in some case, more expensive alternatives.
Though the odd contrast may not be easily seen, there is an argument that erasing PCS in the home may actually cost the tax payers more. Not to mention that erasing PCS in home health would drive agencies bankrupt and staff jobless.
Remember, I have no verification that our General Assembly would or would not eradicate PCS in the home environment. It was mere speculation in a conversation. But the conversation got me thinking about the delicate balance of Medicaid services in NC. And how one abrupt and drastic change could change our health care system and capitalist ideas so quickly.
And, arguably, all because of the speculative “F” word. What is that political phrase we heard so much in the last elections? Oh, yes, maybe we should use a scalpel, not an ax?