Blog Archives
Darkness Surrounds MCO Mergers: Are Closed Meetings for MCOs Legal?
Recently, Eastpointe Human Services’ board voted unanimously to consolidate with Cardinal Innovations Healthcare, which would make the merged entity the managed care organization (MCO) overseeing 1/3 of NC’s Medicaid, behavioral health services – 32 counties, in all.
The Board’s decision is subject to the approval of the Secretary, but Eastpointe hopes to consolidate by July 1st.
Whether a consolidation between Eastpointe and Cardinal is good for Medicaid recipients and/or our community, I have no opinion.
But the reason that I have no opinion is because the negotiations, which all deal with public funds, have occurred behind closed doors.
Generally, it is our public policy that public bodies’ actions are to be conducted openly. This is why you can stroll on over to our courthouse and watch, virtually, any case be conducted. There are rare cases in which the court will “seal” or close the record, such as to protect privileged health information or the identity of children. Our public policy that strongly encourages open sessions for public entities exists for good reason. As tax payers, we expect full disclosure and transparency as to how our tax dollars are being used. In a way, all tax paying NC residents are shareholders of NC. Those who spend our tax dollars owe us a fiduciary duty to manage our tax dollars in a reasonable and responsible manner, and we should be able to attend all board meetings and review all meeting minutes. The MCOs are the agents of the single state entity, Department of Health and Human Services (DHHS), charged with managing behavioral health care for the Medicaid and state-funded population suffering with mental health/developmentally disabled /substance abuse (MR/DD/SA) issues. As an agent of the state, MCOs are public entities.
But, as I am researching the internet in search of Eastpointe and Cardinal board meeting minutes, I realize that the MCOs are initiating closed meetings and quoting N.C. Gen. Stat. § 143-318.11, ” Closed sessions” as the basis for being able to conduct closed sessions. And the number of closed sessions that I notice is not a small number.
The deliberations of a merger between two MCOs are highly important to the public. The public needs to know whether the board members are concerned about improving quality and quantity of care. Whether the deliberations surround a more inclusive provider network and providing more services to those in need. Whether the deliberations consider using public funds to create playgrounds or to fund more services for the developmentally disabled. Or are the board members more concerned with which executives will remain employed and what salaried are to be compensated?
You’ve heard of the saying, “Give him an inch and he’ll take a mile?” This is what is going through my mind as I review the statute allowing public bodies to hold closed sessions. Is the statute too open-ended? Is the closed session statute a legal mishandling that unintentionally, and against public policy, allows public meetings to act privately? Or are the MCOs misusing the closed session statute?
So I ask myself the following:
1. Is N.C. Gen. Stat. § 143-318.11 applicable to MCOs, or, in other words, can the MCOs conduct closed sessions? and, if the answer to #1 is yes, then
2. Are the MCOs overusing or misusing its ability to hold closed sessions? If the answer to #3 is yes, then
3. What can be done?
These are the three questions I will address in this blog.
Number one:
Is N.C. Gen. Stat. § 143-318.11 applicable to MCOs, or, in other words, can the MCOs conduct closed sessions?
According to the statute, “”public body” means any elected or appointed authority, board, commission, committee, council, or other body of the State, or of one or more counties, cities, school administrative units, constituent institutions of The University of North Carolina, or other political subdivisions or public corporations in the State that (i) is composed of two or more members and (ii) exercises or is authorized to exercise a legislative, policy-making, quasi-judicial, administrative, or advisory function.”
The MCOs are bodies or agents of the state that are composed of more than 2 members and exercises or is authorized to exercise administrative or advisory functions to the extent allowed by the Waivers.
I determine that, in my opinion, N.C. Gen. Stat. § 143-318.11 is applicable to the MCOs, so I move on to my next question…
Number two:
Are the MCOs overusing or misusing its ability to hold closed sessions?
As public policy dictates that public bodies act openly, there are enumerated, statutory reasons that a public body may hold a closed session.
A public body may hold a closed session only when a closed session is required:
- “To prevent the disclosure of information that is privileged or confidential pursuant to the law of this State or of the United States, or not considered a public record within the meaning of Chapter 132 of the General Statutes.
- To prevent the premature disclosure of an honorary degree, scholarship, prize, or similar award.
- To consult with an attorney employed or retained by the public body in order to preserve the attorney-client privilege between the attorney and the public body, which privilege is hereby acknowledged. General policy matters may not be discussed in a closed session and nothing herein shall be construed to permit a public body to close a meeting that otherwise would be open merely because an attorney employed or retained by the public body is a participant. The public body may consider and give instructions to an attorney concerning the handling or settlement of a claim, judicial action, mediation, arbitration, or administrative procedure. If the public body has approved or considered a settlement, other than a malpractice settlement by or on behalf of a hospital, in closed session, the terms of that settlement shall be reported to the public body and entered into its minutes as soon as possible within a reasonable time after the settlement is concluded.
- To discuss matters relating to the location or expansion of industries or other businesses in the area served by the public body, including agreement on a tentative list of economic development incentives that may be offered by the public body in negotiations, or to discuss matters relating to military installation closure or realignment. Any action approving the signing of an economic development contract or commitment, or the action authorizing the payment of economic development expenditures, shall be taken in an open session.
- To establish, or to instruct the public body’s staff or negotiating agents concerning the position to be taken by or on behalf of the public body in negotiating (i) the price and other material terms of a contract or proposed contract for the acquisition of real property by purchase, option, exchange, or lease; or (ii) the amount of compensation and other material terms of an employment contract or proposed employment contract.
- To consider the qualifications, competence, performance, character, fitness, conditions of appointment, or conditions of initial employment of an individual public officer or employee or prospective public officer or employee; or to hear or investigate a complaint, charge, or grievance by or against an individual public officer or employee. General personnel policy issues may not be considered in a closed session. A public body may not consider the qualifications, competence, performance, character, fitness, appointment, or removal of a member of the public body or another body and may not consider or fill a vacancy among its own membership except in an open meeting. Final action making an appointment or discharge or removal by a public body having final authority for the appointment or discharge or removal shall be taken in an open meeting.
- To plan, conduct, or hear reports concerning investigations of alleged criminal misconduct.
- To formulate plans by a local board of education relating to emergency response to incidents of school violence or to formulate and adopt the school safety components of school improvement plans by a local board of education or a school improvement team.
- To discuss and take action regarding plans to protect public safety as it relates to existing or potential terrorist activity and to receive briefings by staff members, legal counsel, or law enforcement or emergency service officials concerning actions taken or to be taken to respond to such activity.”
Option 1 clearly applies, in part, to privileged health information (PHI) and such. So I would not expect that little Jimmy’s Medicaid ID would be part of the board meeting issues, and, thus, not included in the minutes, unless his Medicaid ID was discussed in a closed session.
I cannot fathom that Option 2 would ever be applicable, but who knows? Maybe Alliance will start giving out prizes…
I would assume that Option 3 is used most frequently. But notice:
“General policy matters may not be discussed in a closed session and nothing herein shall be construed to permit a public body to close a meeting that otherwise would be open merely because an attorney employed or retained by the public body is a participant.”
Which means that: (1) the closed session may only be used to talk about specific legal strategies and not general policies. For example, arguably, an MCO could hold a closed session to consult with its attorney whether to appeal a specific case, but not to discuss whether, generally, the MCO intends to appeal all unsuccessful cases.
and
(2) the MCO cannot call for a closed session “on the fly” and only because its attorney happens to be participating in the board meeting.
As I am rifling through random board meeting minutes, I notice the MCO’s attorney is always present. Now, I say “always,” but did not review all MCO meeting minutes. There may very well be board meetings at which the attorneys don’t attend. However, the attorney is present for the minutes that I reviewed.
Which begs the question…Are the MCOs properly using the closed sessions?
Then I look at Options 4, and 5, and 6, and 7, and 8, and 9…and I realize, Geez, according to one’s interpretation, the statute may or may not allow almost everything behind closed doors. (Well, maybe not 9). But, seriously, depending on the way in which each Option is interpreted, there is an argument that almost anything can be a closed session.
Want to hold a closed session to discuss why the CEO should receive a salary of $400,000? N.C. Gen. Stat. § 143-318.11(5)(ii).
Want hold a closed session to discuss the anonymous tip claim that provider X is committing Medicaid fraud? N.C. Gen. Stat. § 143-318.11(7).
Want to hold a closed session to discuss how an MCO can position itself to take over the world? N.C. Gen. Stat. § 143-318.11(4).
In an atmosphere in which there is little to no supervision of the actions of the MCOs, who is monitoring whether the MCOs are overusing or misusing closed sessions?
Number three:
What can you do if you think that an MCO is holding closed sessions over and above what is allowed by N.C. Gen. Stat. § 143-318.11?
According to N.C. Gen. Stat. § 143-318.16A, “[a]ny person may institute a suit in the superior court requesting the entry of a judgment declaring that any action of a public body was taken, considered, discussed, or deliberated in violation of this Article. Upon such a finding, the court may declare any such action null and void. Any person may seek such a declaratory judgment, and the plaintiff need not allege or prove special damage different from that suffered by the public at large.”
Plus, according to N.C. Gen. Stat. § 143-318.16A, “[w]hen an action is brought pursuant to G.S. 143-318.16 or G.S. 143-318.16A, the court may make written findings specifying the prevailing party or parties, and may award the prevailing party or parties a reasonable attorney’s fee, to be taxed against the losing party or parties as part of the costs. The court may order that all or any portion of any fee as assessed be paid personally by any individual member or members of the public body found by the court to have knowingly or intentionally committed the violation; provided, that no order against any individual member shall issue in any case where the public body or that individual member seeks the advice of an attorney, and such advice is followed.”
In sum, if you believe that an MCO is conducting a closed session for a reason not enumerated above, then you can institute a lawsuit and request attorneys’ fees if you are successful in showing that the MCO knowingly or intentionally committed the violation.
We should also appeal to the General Assembly to revise, statutorily, more narrowly drafted closed session exceptions.
BREAKING: House and Senate appear close to a Medicaid deal!!
In our last post on Medicaid reform, we updated you on the recent bill passed by the North Carolina Senate relating to the long-standing thorn in the side of the General Assembly, especially regarding the states’ budget – the Medicaid program. The Senate’s version of Medicaid reform is quite different from what we have previously seen and is a hodge-podge of managed care and a new idea: “provider-led entities.”
In a strong sign that this proposal is a compromise between competing sides that could end up getting passed, both House and Senate leaders are speaking positively on the record to news media about the prospects for a deal. Given how public the issue is and how big it is (an expected $14.2 billion in North Carolina in the coming year), that means they expect to get a deal done soon. The fact that the issue is so tied up with the budget that is overdue to be passed is a further headwind to passing a bill.
Right now, the bill is in a conference committee of negotiators from the House and Senate to work out an agreement, given the differences between the two chambers.
One major issue that the committee needs to look at is whether there will be a whole new state agency: the “Department of Medicaid.” The Senate endorsed that idea last week.
Our prediction: The legislators will chart a cautious course and not erect a whole new agency at the same time they are overhauling the system.
With Wos having (coincidentally?) just stepped down as Secretary of the Department of Health and Human Services, perhaps the lack of a lightning rod for criticism of DHHS will let the air out of the proposal to remove Medicaid from DHHS’s hands.
Stay tuned.
By Robert Shaw
The Nine Habits of a Highly Effective Secretary for DHHS
With the recent passing of the torch from Aldona Wos to Rick Brajer (see blog), I’ve been thinking about…
What are the qualifications of a Secretary of DHHS?
What exactly are the qualities that would make a great Secretary of DHHS? Remember, in Mary Poppins, when the children draft their requirements for a nanny? Or, better yet, what are the “Seven Habits of a Highly Effective” Secretary for DHHS? Or…in this case, the “Nine Habits”…
Here are my “Nine Habits of a Highly Effective Secretary of DHHS;” our Secretary of DHHS should have the following:
- A health care background
- A successful track record of his/her ability to manage large companies or agencies
- An understanding of the Medicaid system, and, maybe, even have first-hand knowledge of how the system affects recipients and providers
- A relationship with someone on Medicaid or a parent of someone on Medicaid
- A working knowledge of clinical coverage policies, reimbursement rates, and regulations surrounding Medicaid
- Both the capacity to listen and speak and do both eloquently and genuinely
- True empathy about the physical and mental health of Medicaid recipients and about providers, plus have the patience to handle all types of demographic differences
- An understanding that he/she is handling tax payers’ money, that redundancy in staff is excess administrative costs, and ability to trim the fat
- An ability to communicate with both the Senate and the House and to be frank with both
Let us analyze the qualifications of Wos that we came to witness over the last few years, as well as, review the qualifications of soon-to-be Sec. Brajer with information to which we are privy.
Let’s see if both, either, or neither have these “Nine Habits of a Highly-Effective Secretary for DHHS.”
- Health care background:
Wos: Yes. And, yet, maybe not. She is an M.D. Although I do not know whether she ever practiced medicine in North Carolina. According to Wikipedia, (which is never wrong) Wos “prides herself on her work in the field of preventing HIV and AIDS.” However, I was unable to find a single clinic in which Wos provided services. While, generally, an “M.D.” automatically bestows a certain aura of understanding health care, I question whether this “M.D.” automatically has a working knowledge of billing for and receiving reimbursements under Medicaid in North Carolina.
Brajer: Hmmmm. This one is more tricky. The two companies that Brajer owned, Pro-nerve LLC and LipoScience Inc., are health care related, in that Pro-nerve was an intraoperative neuromonitoring (IONM) company and LipoScience sold a diagnostic tool to health care providers. Arguably, both companies are health care related, at least, in an ancillary way. However, Brajer is not a health care professional, and, to my knowledge, has never rendered health care services. Furthermore, neither of Brajer’s companies was successful; quite the opposite is true, in fact. From my understanding, one company declared bankruptcy and the other was not far behind. Which brings us to the next category…
Answer: Both…kinda.
2. A successful track record of his/her ability to manage large entities:
Wos: Prior to acting as the Secretary to DHHS, Wos served as the Ambassador to Estonia until 2006. What she did besides political functions between 2006 and 2012, I do not know. Acting as an Ambassador does not entail managing large entities. The most managerial skills that I can find in her background, prior to being appointed Secretary, are related to political fund-raising. Since I would not call her brief reign as Secretary of DHHS a success, I give Wos a “two thumbs down” on this criterion.
Brajer: He managed two companies. We can bicker as to whether these companies should be considered large…neither employed 17,000 employees. Regardless, the “successful” criterion appears to be lacking.
Answer: Neither…pickles.
3. An understanding of the Medicaid system:
Wos: “You’re asking me without having all the data available to answer a question,” she told lawmakers on October 8, 2013. In her defense, she responded as such when asked whether the State was moving toward privatization for Medicaid. No one could know the answer, except, maybe, McCrory.
On the other hand, the implementation of NCTracks was nothing short of a catastrophe of epic proportion. See blog. See blog. Anyone with nominal knowledge of the Medicaid system would have, at least, paused to consider keeping HP Enterprises under contract during the switch to NCTracks or pushed back the go-live date.
Brajer: Unknown
Answer: Here’s to hoping that Brajer does. I’m cheering for you! Go! Fight! Win!
4. A relationship with someone on Medicaid or a parent of someone on Medicaid:
Wos: Unknown. If I were shaking a proverbial “8 Ball,” it would read, “Doubtful.”
Brajer: Unknown. Perhaps one of his former employees at Pro-nerve, LLC and LipoScience, Inc. is on Medicaid.
Answer: Gimme a ‘B’! B! Gimme a ‘R’! R! Gimme a ‘A’! A! Gimme a ‘J’! J! Gimme a ‘E’! E! Gimme a ‘R’! R! Whats that spell? Brajer!!
5. A working knowledge of clinical coverage policies, reimbursement rates, and regulations surrounding Medicaid.
Wos: Unknown. Whatever Wos’ knowledge of regulations and clinical coverage policies is or lacked, she, initially, made up for any knowledge lacked with the key hire and quick resignation of Carol Steckel. Unfortunately, Steckel’s experience was never replaced.
January 2013: “I am pleased to say that we are already taking steps to address some of these issues,” Wos said. “Now, the most important of this is that we have hired Ms. Carol Steckel, a nationally recognized — nationally recognized — expert in Medicaid to run our Medicaid program for the state. Carol is already moving ahead with systemic reviews of operations in this division. She is reviewing and establishing new policies and procedures.”
September 27, 2013: Steckel resigns. And blog.
Brajer: Unknown.
Answer: B! R! A! J! E! R! Let’s go, Brajer!
6. Both the capacities to listen and speak and do both eloquently.
Wos: Wos brandished an ability to speak publicly with ease. Listening, on the other hand….eh?
Brajer: Unknown
Answer: I think you can, I think you can, I think you can…
7. Genuine concern about the physical and mental health of Medicaid recipients AND about providers PLUS have the patience to handle all types of demographic differences
Wos: She seems to think so. Her country club does not discriminate.
Brajer: Unknown
Answer: Go! Go! Go! Go! Go, Brajer!!
8. An understanding that he/she is handling tax payers money and that redundancy in staff is excess administrative costs and trim the meat
Wos: “My obligation as secretary is to find the best possible team in order to get the job done.” Les Merritt served as CFO of DMA on a $300,000-plus contract. Joe Hauck was paid over $228,000 for 6 months of advise to Wos. Matt McKillip was paid $87,500 to serve as chief policy maker without any health care background. Ricky Diaz pulled in $85,000 as communications director. Id. Wos has handed out $1.7 million in pay hikes to 280 staffers, many with “no career or educational experience for the jobs they hold.” Id. The implementation of the MCOs also fell under Wos’ watchful eye. The MCO system has created thousands upon thousands of high-paying jobs with our Medicaid dollars. I believe that in the “trim the fat” category, Sec. Wos scores a goose egg.
Brajer: Unknown.
Answer: Please, Brajer! For the love of Pete!
9. Ability to communicate with both the Senate and the House and to be frank with both.
Wos: “Separation pay” v. “Severance pay?”
In April 2013: “I think the word transparency can get pretty dangerous,” Wos said. “Because what does transparency mean? If transparency means that we’re in a planning process and you’re asking us, ‘Tell us all the things you’re planning,’ well, my goodness, allow us to work, and then we’ll give you everything that you want.”
Brajer: Unknown
Answer: Brajer, Brajer, He’s our man! If he can’t do it…[gulp].
____________________________________________
It concerns me that so many of future Sec. Brajer’s core abilities/habits to run and manage DHHS and the Medicaid program in a highly effective manner are unknown. Nothing like placing all your money on red! But we have HIGH hopes for Brajer!!! Don’t let us down!!
The whole point of this blog is to pause and really contemplate what characteristics would comprise a great Secretary for DHHS. Obviously, the Governor has the full authority to appoint the Secretary, meaning that we taxpayers have little to no input as to whether we deem a person qualified, except in the indirect method of voting or not voting for the Governor.
Call this blog an exercise in examining what habits, if in existence, would make the most highly effective Secretary of DHHS and an opinion as to whether these habits exist in our former and future Secretaries.
We are cheering for Brajer! But…
One fact about the future is that it is unknown.
North Carolina Medicaid Reform Update – Round and Round She Goes
Given how long the Medicaid reform discussions have been going on at the legislature, you may be glazed over by now. Give me the memo when they pass something, right? Fair enough, let’s keep it brief. Where do things stand right now?
Last Wednesday, the Senate staked out its position in the ongoing debate between the House and the McCrory administration.
The Senate’s newest proposal is an unusual mix of different systems and new ideas. Not willing to commit to one model for the whole Medicaid program, the latest version of the bill includes something new called Provider Led Entities, or “PLEs.” PLEs are yet the latest in the alphabet soup of different alternatives to straight fee-for-service billing for Medicare/Medicaid. You’ve all heard of HMOs, PPOs, MCOs, and ACOs. PLEs appear to be similar to ACOs, but perhaps for political reasons the Senate bill sponsors saw the need to call the idea something different. See Knicole Emanuel’s blog.
In any event, as the name suggests, such organizations would be provider-led and would be operated through a capitated system for managing the costs of the Medicaid program. The Senate bill would result in up to twelve PLEs being awarded contracts on a regional basis.
PLEs are not the only addition to the Medicaid alphabet soup that the Senate is proposing in its version of HB 372. The Senate has also renewed its interest in taking Medicaid out of the hands of the N.C. Department of Health and Human Services entirely and creating a new state agency, the Department of Medicaid (“DOM”).
(One wonders whether the continual interest in creating a new Department of Medicaid independent of the N.C. Department of Health and Human Services had anything to do with embattled DHHS Secretary Wos stepping down recently.)
The Senate also proposes creating a Joint Legislative Oversight Committee on Medicaid (“LOC on Medicaid”).
But creating the DOM and using new PLEs to handle the provision of Medicaid services is not the whole story. Perhaps unwilling to jump entirely into a new delivery system managed by a wholly new state agency, the Senate bill would keep LME/MCOs for mental health services in place for at least another five years. Private contractor MCOs would also operate alongside the PLEs. The North Carolina Medicaid Choice coalition, a group which represents commercial MCOs in connection with the Medicaid reform process, is pleased.
One very interesting item that the Senate has included in its proposed legislation is the following requirement: “Small providers shall have an equal opportunity to participate in the provider networks established by commercial insurers and PLEs, and commercial insurers and PLEs shall apply economic and quality standards equally regardless of provider size or ownership.” You can thank Senator Joel Ford of Mecklenburg County for having sponsored this amendment to the Senate version of House Bill 372.
By pulling the Medicaid reform proposal out of the budget bill, the matter appears headed for further negotiation between the House and the Senate to see if the two can agree this year, unlike last year.
By legislative standards, that counts as forward progress… Here come the legislative discussion committees to hash it out more between the two chambers. We will keep a close eye on the proposals as they continue to evolve.
By Robert Shaw

Passing the Torch: Wos Resigns!! Brajer Appointed!
Aldona Wos resigned today after two years and seven months as Secretary of NC DHHS. Wos’ last day will be Aug. 14.
McCrory named Rick Brajer, a former medical technology executive, as the new Secretary of DHHS.
Soon-to-be Sec. Brajer, 54, was the chief executive of ProNerve and LipoScience. LipoScience was sold to LabCorp in 2014, and ProNerve was sold to Specialty Care in April.
Brajer is not a doctor, as Wos was. Instead, Brajer touts an MBA from Stanford.
I do not have any information as to why Wos resigned now, especially in light of the recent resignation of the Secretary of Transportation, but will keep you apprised.
More to come….
Consider Nominating This Blog for the 2015 Best Legal Blog Contest (Please)!
The 2015 Legal Blog Contest is here!
For all you that follow this blog, thank you! I hope that you agree that I provide you with valuable and up-to-date information on Medicaid/care regulatory issues. At least, that is my hope in maintaining this blog. And maintaining this blog takes a lot of time outside my normal, hectic legal career and my time as a mom and wife. Don’t get me wrong…I love blogging about these issues because these issues are near and dear to my heart. I am passionate about health care, health care providers, Medicaid and Medicare, and access to quality care.
If you are a follower, then you know that I try to keep my readers current on Medicaid/care fraud, federal and state laws, legal rights for health care providers, bills in the General Assembly germane to health care, extrapolation issues, CMS rulings, managed care matters, reimbursement rates, RAC audits and much, much more!
If you enjoy my blog, I ask a favor. Please consider nominating my blog for the 2015 Best Legal Blog Contest.
If you want to nominate my blog, please click here.
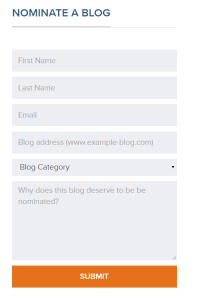
Scroll down until you see this:
Enter your name, email address, my blog address. which is:
For category, click on “Niche and Specialty.” I do not believe the other categories correctly describe my blog.
And type a reason why you enjoy my blog. Much appreciated!

State Auditor Finds Robeson County School NOT Using Medicaid Money
Our State Auditor Beth Wood’s most recent audit finds that The Public Schools of Robeson County failed to spend approximately $1 million in Medicaid dollars intended for special needs children in schools!!
See audit report.
“The Public Schools of Robeson County (School District) did not use approximately $1 million per year in Medicaid administrative reimbursements to provide required services to students with disabilities. The School District missed this opportunity to better serve students with disabilities because it was unaware of a contractual requirement to use the Medicaid reimbursements to provide required services.
…
Over the last three years, the School District reported that it used $26,780 out of $3.16 million in Medicaid administrative reimbursements to provide services to students with disabilities.
The amounts reportedly spent each year are as follows:
• $ 8,969 out of $1,010,397 (0.89%) in 2013
• $12,043 out of $872,299 (1.38%) in 2012
• $ 5,768 out of $1,278,519 (0.45%) in 2011”
The question that I have after reading the audit report is…WHERE IS THE MONEY?
Was this $1 million given to the school system and spent on items other than services for children? Is the school district sitting on a surplus of money that was unspent? Or was this amount budgeted to the school system and the remainder or unspent money is sitting in our state checking account?
To me, it is relatively unclear from the audit report which of the above scenarios is an accurate depiction of the facts. If anyone knows, let me know.
MCO CEO Compensated $400,000 Plus Bonuses with Our Tax Dollars!
On July 1, 2014, Cardinal Innovations, one of NC’s managed care organizations (MCOs) granted its former CEO, Ms. Pam Shipman, a 53% salary increase, raising her salary to $400,000/year. In addition to the raise, Cardinal issued Ms. Shipman a $65,000 bonus based on 2013-2014 performance.
$400,000 a year, plus bonuses. Apparently, I got into the wrong career; the public sector seems to pay substantially more.
Then in July 2015, according to the article in the Charlotte Observer, Cardinals paid Ms. Shipman an additional $424,975, as severance. Within one year, Ms. Shipman was paid by Cardinal a whopping $889,975. Almost one million dollars!!!! To manage 16 counties’ behavioral health care services for Medicaid recipients.
For comparison purposes, the President of the United States earns $400,000/year (to run the entire country). Does the CEO of Cardinal equate to the President of the United States? Like the President, the CEO of Cardinal, along with all the other MCOs’ CEOs, are compensated with tax dollars.
Remember that the entire purpose of the MCO system is to decrease the risk of Medicaid budget overspending by placing the financial risk of overspending on the MCO instead of the State. In theory, the MCOs would be apt to conservatively spend funds and more carefully monitor the behavioral health care services provided to consumers within its catchment area to ensure medically necessity and not wasteful, unnecessary services.
Also, in theory, if the mission of the MCOs were to provide top-quality, medically necessary, behavioral health care services for all Medicaid recipients in need within its catchment area, as the MCOs often tout, then, theoretically, the MCOs would decrease administrative costs in order to provide higher quality, beefier services, increase reimbursement rates to incentivize health care providers to accept Medicaid, and maybe, even, not build a brand, new, stand-alone facility with top-notch technology and a cafeteria that looks how I would imagine Googles’ to look.
Here is how Cardinal’s building was described in 2010:
This new three-story, 79,000-square-foot facility is divided into two separate structures joined by a connecting bridge. The 69,000-square-foot building houses the regional headquarters and includes Class A office space with conference rooms on each floor and a fully equipped corporate board room. This building also houses a consumer gallery and a staff cafe offering an outdoor dining area on a cantilevered balcony overlooking a landscaped ravine. The 10,000-square-foot connecting building houses a corporate training center. Computer access flooring is installed throughout the facility and is supported by a large server room to maintain redundancy of information flow.
The MCOs are not private companies. They do not sell products or services. Our tax dollars comprise the MCOs’ budget. Here is a breakdown of Cardinal’s budgetary sources from last year.
The so-called “revenues” are not revenues; they are tax dollars…our tax dollars.
78.1% of Cardinal’s budget, in 2014, came from our Medicaid budget. The remaining 21.7% came from state, federal, and county tax dollars, leaving .2% in the “other” category.
Because Cardinal’s budget is created with tax dollars, Cardinal is a public company working for all of us, tax paying, NC, residents.
When we hear that Tim Cook, Apple’s CEO, received $9.22 million in compensation last year, we only contributed to his salary if we bought Apple products. If I never bought an Apple product, then his extraordinarily high salary is irrelevant to me. If I did buy an Apple product, then my purchase was a voluntary choice to increase Apple’s profits, or revenues.
When we hear that Cardinal Innovations paid $424,975 to ousted CEO, Pam Shipman, over and above her normal salary of $400,000 a year, we all contributed to Shipman’s compensation involuntarily. Similarly, the new CEO, Richard Toppings, received a raise when he became CEO to increase his salary to $400,000 a year. Again, we contributed to his salary.
A private company must answer to its Board of Directors. But an MCO, such as Cardinal, must answer to tax payers.
I work very hard, and I expect that my dollars be used intelligently and for the betterment of society as a whole. Isn’t that the purpose of taxes? I do not pay taxes in order for Cardinal to pay its CEO $400,000.
For better or for worse, a large percentage of our tax dollars, here in NC, go to the Medicaid budget. I would venture that most people would agree that, as a society, we have a moral responsibility to ensure that our most vulnerable population…our poorest citizens…have adequate health care. No one should be denied medical coverage and our physicians cannot be expected to dole out charity beyond their means.
Hence, Medicaid.
We know that Medicaid recipients have a difficult time finding physicians who will accept Medicaid. We know that a Medicaid card is inferior to a private payor card and limits provider choice and allowable services. We know that certain services for which our private insurances pay, simply, are not covered by Medicaid. Why should a Medicaid-insured person receive sub-par medical services or have more difficulty finding willing providers, while privately insured persons receive high quality medical care with little effort? See blog or blog.
Part of the trouble with Medicaid is the low reimbursements given to health care providers. Health-care consulting firm Merritt Hawkins conducted a study of Medicaid acceptance rates which found that just 45.7 percent of physicians are now accepting Medicaid patients in the U.S.’s largest 15 cities and the numbers worsen when you look at sub-specialties.
The reimbursement rates are so low for health care providers; the Medicaid services are inadequate, at best; and people in need of care have difficulty finding Medicaid physicians. Yet the CEO of Cardinal Innovations is compensated $400,000 per year.
Cardinal has 635 employees. Its five, top-paid executives are compensated $284,000-$400,000 with bonuses ranging $56,500-$122,000.
Richard Topping, Cardinal’s new CEO, told the Charlotte Observer that “it doesn’t cut into Medicaid services.”
He was also quoted as saying, “It’s a lot of money. It is. You’ve just got to look at the size and the scope and the scale.”
In contrast, Governor McCrory is compensated approximately $128,000. Is McCrory’s “size, scope, and scale” smaller than the CEO’s of Cardinal? Is the CEO of Cardinal “size and scope and scale,” more akin to the President of the US?
“We are a public entity that acts like a private company for a public purpose,” Toppings says. Each MCO’s Board of Directors approve salaries and bonuses.
Cardinal is not the only MCO in NC compensating its CEO very well. However, according to the Charlotte Observer, Cardinal’s CEO’s compensation takes the cake.
Smokey Mountain Center (SMC) pays its Chief Medical Officer Craig Martin $284,000 with a $6,789 longevity bonus.
Four years ago, before the initial 11 MCOs, the administrative cost of the MCOs was nonexistent (except for the pilot program, Piedmont Behavioral Health, which is Cardinal now). Implementing the MCO system increased administrative costs, without question. But by how much? How much additional administrative costs are acceptable?
Is it acceptable to pay $400,000+ for a CEO of a public entity with our tax dollars?
NC State Auditor Finds Eastpointe Guilty of Accepting Kickbacks!
Last week I traveled to Houston, Dallas, and Denver to meet with other health care attorneys of Gordon & Rees. It was a great trip and I met some wonderful colleagues. But I was happy to get home to my family, including our new addition of 9 peacock eggs.
Yes, 9 peacock eggs!!
Here is a pic:
(I know that there are 10 eggs in the picture, but we will not talk about the 10th. Just know that we have high hopes that the other 9 are viable and survive!! As of today, at 1:00 pm, all 9 eggs are chirping, but no cracks yet!!)
Oh, and, before I forget…Watch ABC news tonight. I was interviewed for a story about one of my clients.
Anyway, while I was gone, I was unable to post a blog regarding the State Auditor’s most recent audit report regarding Eastpointe. So here it is…
As the managed care organizations (MCOs) continue to accuse health care providers of fraud, waste, and abuse (FWA), it seems from a recent State Auditor report that, at least, one of the MCOs itself is guilty of the very accusation that they are alleging against providers. See blog. And blog.
There is an old story:
A wolf, passing by, saw some shepherds in a hut eating for their dinner a haunch of mutton. Approaching them, he said: What a clamor you would raise, if I were to do as you are doing!
Moral:
Men are too apt to condemn in others the very things they practice themselves
The audit findings beg the questions…Is it only Eastpointe? Or all 9 MCOs? How much Medicaid money is lining the pockets of MCO executives, instead of paying for medically necessary services for Medicaid recipients? Beth Wood only audited Eastpointe. Is this only the tip of the iceberg?
According to our State Auditor, Eastpointe former executive has lined his pockets with $547,595+…
Here are the key findings from the NC State Auditor’s report regarding Eastpointe:
KEY FINDINGS
- Former CFO facilitated apparent kickbacks totaling $547,595 from two Eastpointe contractors
- Former CFO purchased three vehicles totaling $143,041 without a documented business purpose
- Former CFO purchased $18,600 of equipment for personal use
- Former CFO, Chief Executive Officer (CEO), and other employees used Eastpointe credit cards to make $157,565 of questionable purchases
- Inadequate CEO and area board oversight contributed to operational failures
Eastpointe is one of 9 MCOs in NC charged with managing and supervising Medicaid behavioral health care services. So what do we do when the entity IN CHARGE of managing Medicaid money is mismanaging tax dollars???
Where is the supervision??
Over the last few years, since the MCOs went live across the state, I have seen the MCOs terminate Medicaid providers for no cause, claim providers owed money, penalties, plans of corrections (POC), and/or refuse to contract with providers for reasons as silly as:
- Failing to put shoes on a paraplegic (no feet), because the assessment included that the patient required help dressing;
- Using green ink (a personal favorite) on a service note;
- Having signatures on service notes that are difficult to read (so the auditors assume that the person doesn’t have the correct licenses).
Here, we have the State Auditor finding that Eastpointe’s former CFO unilaterally hired two contractors to improve Eastpointe’s building (paid for with Eastpointe’s funding), but the former CFO accepting over half a million dollars. This is no green ink! This is no insignificant finding!!
What is Eastpointe’s funding?
As you can see, 72.7% of Eastpointe’s funding is pure Medicaid money. When Eastpointe’s former CFO received $547,595 in kickbacks, 72%, or $394,268.40, should have been used to provide Medicaid behavioral health care services.
These are our tax dollars, people!! These are our tax dollars budgeted to aid our most needy population with behavioral health care services!! These are our tax dollars budgeted to provide psychiatric services, substance abuse services, and services for those with developmental disabilities!!!!
Our State Auditor states in her report, “The former CFO may have violated several state laws including fraud, misrepresentation, and obtaining property by false pretenses.”
Let’s look at a couple of those statutes that may have been violated:
42 U.S. Code § 1320a–7b imposes criminal penalties for acts involving Federal health care programs, and federal dollars pay a portion of our Medicaid program.
North Carolina General Statute § 14-234 states: “No public officer or employee who is involved in making or administering a contract on behalf of a public agency may derive a direct benefit from the contract except as provided in this section, or as otherwise allowed by law.”
The question becomes was the former CFO of Eastpointe, at the time of the receipt of kickbacks a “public officer” or “employee who is involved in making or administrating a contract on behalf of a public agency?” I believe the answer is yes, at least as to the latter.
Here is the point in this blog that my personal views will be aired. I find the former CFO’s behavior significantly opprobrious and reprehensible.
Here we have an MCO which is in charge of behavioral health care for our most vulnerable and needy populations…not just those in poverty, but those in poverty suffering from mental illness, substance abuse, and/or developmental disabilities (MH/SA/DD). Obviously, those Medicaid recipients suffering from MH/SA/DD will not have the means to hire a private attorney to defend their interests. When they receive denials for authorizations or reductions in services, they are defenseless. Sure, some children have strong advocate parents, but, on the whole, those suffering from MH/SA/DD have little to no advocates.
Juxtapose someone sitting in the role of a CFO…a chief financial officer of a company. Think he or she can hire a private attorney?? Think he or she has advocates or means to hire advocates??
How can someone in power abuse that power to the detriment of the under-privileged and sleep at night? I find the State Auditor’s audit findings repugnant beyond comprehension.
We are left with a former CFO who may or may not have committed criminal activity, but, who, at least according to the State Auditor, has received kickbacks. We are left with questions.
Is it only Eastpointe? Or all 9 MCOs? How much Medicaid money is lining the pockets of MCO executives, instead of paying for medically necessary services for Medicaid recipients? Will there be justice?
We can only hope that this audit is a catalyst to consequences.
NC MCOs and Consolidation: “When the Music Stops? Nobody Knows!”
Our General Assembly is pushing for the managed care organizations (MCOs) to consolidate and/or morph. Consolidating the MCOs makes fiscal sense for our state, but if I were executive management at an MCO, I would be be anxiously awaiting direction from our General Assembly. A metaphoric 3-4 chair game of”Musical Chairs” is proceeding with 9 (now 8) players. Five to six players will have no chairs when the music stops.
What are MCOs? See blog and blog.
Multiple bills have been proposed.
Senate Bill 703 proposes 3 statewide MCOs. Senate Bill 574 seems to incorporate provider-led capitated health plans, but is unclear as to the exact model. Senate Bill 696 seems to create a symphony of provider-led and nonprovider-led, risk-based entities. Senate Bill 568 contemplates licensed commercial health insurers offering health care plans.
No one really knows how many MCOs will remain in the end…if any. Regardless, what the number of existing MCOs in the future will be, there is little dispute that the number will be fewer than the number of MCOs that exist now.
In an atmosphere where there is supposition that there are too many people or companies and that only a few will remain, competition brews. People/companies are forced to strategize if they want to survive.
Think about the childhood game, “Musical Chairs.” You start with a large group of people, but with one less chair than the number of people. The music plays and the players meander around at a relatively slow pace, around and around, until the music stops. And what happens when the music stops? The people scramble for a chair. The person left standing is “out” and must sit on the sideline.
We have 9, soon to be 8, MCOs in NC right now. And the music is playing. But which MCOs will be left standing when the music stops?
Here is a map of our current MCOs:
As of July 1, CoastalCare and East Carolina Behavioral Healthcare (ECBH) will be merged. We will be down to 8 MCOs. Which means that the light blue on the bottom right hand side of the map will merge with the bright yellow on top right hand side of the map.
Mecklenburg county, which houses most of the Charlotte area, was not always light purple. It recently merged with Cardinal Innovations.
Partners (light yellow) and Smokey Mountain (dark blue) had serious discussions of a merger until, recently, when both walked away from negotiations of merger.
Why should it matter which MCOs are in existence or how many? Theoretically, it shouldn’t. These MCOs are created in order to manage behavioral health care (Medicaid services for those suffering from substance abuse, mental illness, and developmentally disabled), not to make a profit, right? The only issue of importance should be that medically necessary behavioral health care services are rendered to Medicaid recipients in the most efficient and most effective manner.
Yet competing interests come into play.
Think about it…each MCO employs hundreds of people. Each MCO has a CEO, who is not working for free. Generally, unless other arrangements have been negotiated, there can only be one CEO per MCO. When there are 2+ MCOs merging with 2 CEOs and only 1 “chair” for 1 CEO, it can seem like “Musical Chairs.” Multiple people are vying for one “chair.”
The money at issue for behavioral health care in NC is not a small amount. It is likened to a fire hose spouting money. We have a Medicaid budget in NC of approximately 14 billion dollars. To put it in perspective, with $14 billion dollars, you could purchase the LA Lakers 14 times. This is how much money we spend on Medicaid every year. It is really quite staggering when you think about it.
As every North Carolinian learns in the 6th grade, North Carolina is composed of 100 counties. The estimated Medicaid budget of $14 billion is allocated across 100 counties and among approximately 1.9 million Medicaid recipients.
When it was decided to implement the MCOs across the state, about 2012-ish (we actually obtained permission from CMS for the waiver years prior to 2012, but we began with a pilot and did not implement the MCOs statewide until 2012-13), we found ourselves, initially, with eleven MCOs, and now we have 9…soon to be 8.
The newly merged entity of CoastalCare and ECBH (CC+ECBH) will manage state funds and Medicaid dollars for behavioral health services across 24 counties in eastern North Carolina. In other words almost ¼ of the Medicaid budget will be handed to CC+ECBH, leaving approximately ¾ of the Medicaid budget for 7 other MCOs (the budget is determined by number of recipients, so I am assuming, for the purpose of this blog, that more counties mean more people).
The amount of counties controlled by the remaining 7 MCOs are as follows:
Smokey: 23
Partners: 8
Centerpointe: 4
Cardinal: 16
Sandhills: 9
Eastpointe: 12
Alliance: 4
Looking at the chart above, it would appear that Smoky and CC+ECBH will manage almost 1/2 the state’s behavioral health care for Medicaid.
Prior to the 1915 b/c Waiver allowing the MCOs to manage behavioral services for Medicaid recipients in NC, DHHS managed it. (Obviously ValueOptions and other vendors had a part in it, but not with actual management). As the single state agency for Medicaid, DHHS cannot delegate administrative duties to contracted parties without a “Waiver,” or permission for an exception from the federal government, or, more specifically, the Center for Medicare and Medicaid Services (CMS).
Prior to the 1915 b/c Waiver, we did not have 9 companies with hundreds of employees managing behavioral health care for Medicaid recipients. We had DHHS, which employs approximately 18,000 employees. To my knowledge DHHS did not terminate those employees who were in charge of behavioral health care issues in order to compensate the creation of new companies/employees. In other words, say 1000 people at DHHS devoted their time to issues arising our of behavioral health care. Once we had an additional 9 (well, 11, at first), those 1000 employees were not asked to join the MCOs. Maybe some did, but, to my knowledge, there was no suggestion or incentive or requirement to leave DHHS and go to an MCO (to shift the administrative burden).
When we created an additional 9 (well, 11 at first) companies to, essentially, take over behavioral health care…
We created more administrative costs, in order to lift the risk of overspending the Medicaid budget off the state. It is estimated that America wastes $190 billion in excess administrative costs per year.
In theory, consolidating the MCOs would decrease administrative costs by having fewer paid employees, not dissimilar to why MCOs want a closed network. See blog. Again, in theory, having fewer MCOs may create a more consistent statewide manner in managing behavioral health care.
Assume for the purpose of this blog that each MCO employs 100 people (which is a very low number) and each employee is paid $50,000, then the administrative cost associated with delegating behavioral health care to MCOs equals $500,000, counting only employee salaries. Multiple that number by 9 (number of current MCOs) and you get an increased administrative cost of approximately $4.5 million dollars per year, not counting the additional overhead each MCO bears (rent/mortgage, equipment, salary benefits, health care benefits, etc.). Plus you have to include the top management’s salaries, because you know the executives are receiving more than $50,000/year.
What motivated us to implement a MCOs system? With an MCO system, the General Assembly is able to allocate funds for Medicaid and place the risk of going over the budget on the MCOs, not the state. This is a completely understandable and reasonable objective. It is without question that the Medicaid budget is swelling to the point of unsustainability.
However, are we trading “control/supervision” for “knowability?” Are we also trading “risk” for “higher administrative costs,” which, in turn, equals less Medicaid dollars for providers and Medicaid recipients? Every dollar paid to an MCO employee is a dollar not going to a health care provider to reimburse for services.
For these reasons, the government’s push for consolidation of the MCOs is astute. Fewer MCOs = less administrative costs. Fewer MCOs = easier supervision by DHHS.
Less administrative costs = more Medicaid dollars going to providers…to serve our most needy. Because, at the end of the day, the most important issue when it comes to Medicaid is providing quality care for recipients.
It is no matter which entity controls/manages behavioral health care for Medicaid, because regardless the entity, that entity should be managing our tax dollars in the most efficient way that provides the best quality to services to those in need.
“Around and around we go, when we stop? Nobody knows…” But we do know this…when the music stops, there will be scrambling!